Kidneys II - Tubulointerstitials, Congenital, Adenomas Flashcards
(44 cards)
What are the characteristics of acute tubular necrosis?
multiple etiologies
major cause of acute renal failure
usu reversible (can reconstruct itself to restore functionality- labile)
What are the two broad categories of acute tubular necrosis?
ischemic (patchy necrosis)
nephrotoxic (segmental e.g. proximal convoluted tubule)
Where do we see ischemic ATN?
scattered along length of PCT and loops of Henle - does NOT afect just one focal segment
What are some causes for ischemic ATN?
1) thrombus/embolus
2) massive exsanguinations (GSW, trauma, etc)
3) hypovolemia/shock (blood being shunted away from kidneys)
Where do we see nephrotoxic ATN?
tend to be segmental, or more focal, particularly within PCT
What is unique to nephrotoxic ATN?
sudden onset, which results in coagulative necrosis of renal tubular epithelium
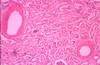
What is this?

ATN
key feature here: cortical pallow (esp. in ischemic subtype)
What is this?

cortical necrosis of ATN- see fibrosis, scarring, and contraction
What’s the treatment for ATN?
vasopressin - to get BP back up and regulate fluid volumes,
make sure kidneys are perfused
dialysis
What are some characteristics of acute pyelonephritis?
bacterial infection (usu gram neg)
ascending or hematogenous routes
associated with urine stasis, obstruction, retrograde flow (cystitis to pyelonephritis)
patchy interstitial suppurative inflammation (microabscesses)
Does acute pyelonephritis start as cortical disease?
NO! as the disease worsens, it can affect the cortex
What is this?

pyuria = pus in urine (so PMNs and RBCs)
NOT pathognomonic
seen in acute pyelonephritis
What is another key feature of acute pyelonephritis?
WBC casts - indicative of inflammation/infection
can potentially have 2 different kinds - renal tubular or epithelial casts

Where do the WBC cast originate from?
ONLY renal tubule- so this means it CANNOT be a lower UTI (has to originate in the kidney itself)
What is shown here?

acute pyelonephritis - enlarged and swollen
microabscesses: tiny yellow dots scattered throughout cortex and medulla (CLASSIC sign of inflammation)
What happens to microabscesses?
will become dropout areas - no longer able to perform renal functions
What is the cause of the flank pain seen in acute pyelonephritis?
stretching of the kidney’s capsule due to the enlargement of the organ secondary to inflammatory mediators and infiltrates
What is shown here?

chronic pyelonephritis
note the grossly scarred kidneys
What causes chronic pyelonephritis?
interstitial fibrosis and atrophy of tubules due to multiple bouts of acute pyelonephritis
toxins or drugs inducing acute immunologic (hypersensitivity) reaction in the interstitium - resulting in interstitial inflammation with predominantly _?_
progression?
Interstitial nephritis
eosinophils ; papillary necrosis
What is seen histologically in TID - Interstitial Necrosis?
- tubules separated (should be back-to-back)
- interstitium full of inflammatory cells
- normal glomeruli
- eosinophils!

What is this?

papillary necrosis - yellowish-softening coagulative necrosis of medullary pyramid papillae
What is this?
What happens when sloughs off?

papillary necrosis!
- get acute onset of anuria (bc the tubes get blocked)- lose ability to concentrate urine
What are the causes of papillary necrosis?
- acute pyelonephritis
- interstitial nephritis
- diabetic nephropathy
- sickle cell disease
- nephrotoxity drugs