Hematology - Hemostasis Flashcards
Coagulation Platelet Activation Hypercoagulable States Coagulopathies Platelet Disorders Antiplatelet Drugs Anticoagulant Drugs (171 cards)
how does the body prevent blood loss when there is damage to a blood vessel?
thrombus formation
platelets are activated and fibrin crosslinks to form a clot
what is the first line of defense against bleeding?
vasoconstriction in response to endothelial damage
mediated by ENDOTHELINS
what are endothelins?
key mediator in the vasoconstrictor compensatory response to prevent blood loss
they are proteins
they are potent vasoconstrictors
they are released by endothelial cells near the damage
what are endothelin receptor blockers used for?
Pulmonary HTN
what are coagulation factors?
proteins synthesized by the liver
soluble in plasma
activated when endothelial damage occurs
forms fibrin => fibrin mesh => blood clot
what form do coagulation factors circulate in?
zymogens
what are serine proteases?
protein cleavage enzyme that contains serine
clotting factors can activate into a serine protease
what are the steps in the clotting cascade?
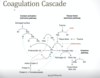
activation of what clotting factor will lead to fibrin formation?
X –> Xa

what drugs act on the clotting cascade?

what is the positive feedback associated with thrombin?
factor IIa activates factors V, XI, VIII
XIa activates IX —> IXa
IXa + VIIIa —> Xa

what activates factor X in the setting of endothelial damage?
tissue factor becomes activated by endothelial damage which interacts with factor VII to activate factor X
TF:VIIa complex activates Xa
what is tissue factor?
aka thromboplastin
glycoprotein expressed in SUBendothelial cells NOT endothelial cells => no contact with citculating blood unless exposed by endothelial damage
what is thrombin?
aka factor IIa
prothrombin is factor II
can activate factors V, XI, VIII
what are the components of extrinsic Xase?
phospholipid: TF-bearing cells
Enzyme: factor VIIa
co-factor: TF
substrate: factor X

what are the unique features of factor VIII?
produced in endothelial cells, not in the liver
circulates bound to vWF
released from vWF in response to vascular injury
what are the components of intrinsic Xase?
phospholipid: platelets
enzyme: factor IXa
co-factor: factor VIII (VIIIa)
substrate: factor X

what is vWF?
von willebrand factor
critical for platelet aggregation
binding to vWF increases VIII plasma half life
what cells produce vWF?
endothelial cells and megakaryocytes
what are the multicomponent complexes that activate X –> Xa?
- Extrinsic Xase
- Intrinsic Xase
what is calciums role in coagulation?
used to be called factor IV - required for the clotting cascade
activated platelets release calcium
EDTA binds calcium in blood samples and prevents clotting
what is the order of the intrinsic pathway?
XII
XI
IX
X
II
I

what is the order of the extrinsic pathway?
TF:VIIa
X
II
I







