Huntington's Disease Flashcards
(19 cards)
Non-motor aspects of Huntington’s disease
- Early in the disease course, personality changes and mild cognitive decline are common
- As disease progresses, cognitive decline continues to dementia and significant psychiatric features (apathy, depression, anxiety) often develop
- Memory is unaffected
Inheritance pattern of Huntington’s disease
Autosomal dominant with paternally-derived anticipation
Motor aspects of Huntington’s disease
- Progressively developing choreiform movements with a SLOW, insidious onset
- Imbalance
- Brisk reflexes
- Dysphagia (late in disease)
Thing that must always be ruled out before making the diagnosis of Huntington’s disease
Medication effect or illicit drug effect
ie, tardive dyskinesia
Best diagnostic test for Huntington’s
Genetic testing
Athetosis
Twisting and writhing movements often associated with chorea. Often in reference to positioning of the fingers/hands. Also seen in cerebral palsy.

What is the sequence repeat in Huntington’s?
CAG
Triplet repeat length and cinical correlation in Huntington’s
- >40 = full penetrance
- 36-39 = incomplete penetrance, uncertain phenoconversion
1 cause of death in Huntington’s patients
Aspiration pneumonia
Due to Huntington’s associated dysphagia
Early history and physical exam signs of Huntington’s
-
History:
- Family history
- Personality change
-
Exam:
- Slowing of saccades
- Hyper-reflexia
- Disinhibition of primitive reflexes
Westphal variant Huntington’s Disease
- aka Juvenile onset Huntington’s
- < 5% of cases
- Presents with hypokinetic movement features often described as parkinsonian, unlike the hyperkinetic features of adult HD
- Hypokinetic: Bradykinesia, rigidity
- Hyperkinetic: Dystonia, myoclonus, seizures
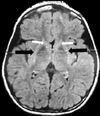
- Imaging: (MRI or CT)
- Bilateral atrophy of the head of the caudate nucleus and putamen
In a child or teenager (ages ~5-15), __ should always be considered as an etiology of choreiform movement disorder
In a child or teenager (ages ~5-15), Sydenham’s chorea should always be considered as an etiology of choreiform movement disorder
Sydenham’s chorea
- The “S” in the JONES criteria for rheumatic fever
- Should be suspected in any case of chorea of a patient 5-15 years of age
- An acute, self-limited choreiform movement disorder caused by infection-associated autoimmunity
- Strongly associated with Group A streptococcus infection
- However, only 30% of patients with Sydenham’s have it due to established rheumatic fever
- Antistreptolysin-O and Anti-DNAse B should be order for all patients to assist diagnosis
- Treatment is usually unnecessary
Treatment for Huntington’s
There is no disease modifying treatment. However, symptomatic treatments are available. These will be discussed separately
Symptomatic treatment for chorea
- Improved w/ drugs that interfere with dopaminergic activity
- Tetrabenazine is the only FDA-approved medication for Huntington’s chorea
- If tetrabenazine is not well tolerated or insufficient, it may be substituted or attenuated by atypical neuroleptics (olanzapine, risperidone)
- If all else fails, haldol is always an option
- Unfurtuantely, if neuroleptics are used to treat HD, it can become unclear whether bradykinesia and rigidity that develop are due to HD itself or a side effect of the dopaminergic antagonists.
- It is not uncommon for these agents to be discontinued as HD progresses
Tetrabenazine
- First-line for HD chorea
- Reversibly depletes monamines from nerve terminals, ultimately decreasing release of dopamine
- May cause or worsen symptoms of depression
___ is an extremely common psychiatric comorbidity of Huntington’s
Depression is an extremely common psychiatric comorbidity of Huntington’s
This is typically treated, like all forms of depression, with SSRIs
Reducing the risk of aspiration in Huntington’s patients
Percutaneous endoscopic gastrostomy (PEG) tubes may be advised early in the disease course in order to provide adequate nutrition and decrease aspiration.
Speech and occupational therapy can also be helpful for this purpose.
Movement affects of long-term dopaminergic antagonist usage
Parkinsonism (acute, dose-dependent)
Tardive dyskinesia (chronic, structural change)


