immunology I Flashcards
(48 cards)
common CBC trend seen in acute bacterial infection
- increased neutrophils
common CBC trend seen in acute parasitic infection
- increased Eosinophils
common CBC trend seen in acute viral infection
- increased lymphoctyes
immunogenicity
the capacity to induce an immune response by foreign, complex, high molecular weight compounds
Antigenicity
ability to bind to Ig or immune cells; an immune response need not result
the site on an antigenat which a specific antibody becomes attached
epitope
a partial antigen; a specific nonprotein substance which does not itself elicit antibody formation but does elicit the immune response when coupled with a carrier protein
hapten
an antibody that reacts with an antigen other than the one that induced its production
cross-reacting antibody
characterizes which immune system:
- rapidly mobilized first line of defense
- not dependent on prior exposure to foreign invader
- non-specific
- response does NOT increase with repeat exposure
innate (natural, native) immune system
describe the “respiratory burst” of innate immune system
- membrane-bound NADPH system produces
- superoxide radicals
- hyperchlorous acid
- H2O2
- chloramines
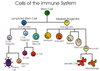
list granulocyte cells that are part of innate immunity
- neutrophil
- eosinophil
- basophil
- mast cell

list components of innate immunity
- macrophages
- granulocytes
- natural killer cells
- complement
- physical barriers
name “Barriers” component of innate immune system
- skin
- commensal bacteria: normal bacterial flora
- compete with potential pathogens
- mucous membranes
- tears
- saliva
- mucus
- gastric secretions
what does mucus contain that protects against gram positive bacteria
lysozyme
basophils and mast cells share a progenitor. where does each settle to mature
- basophils mature in the bone marrow
- mast cells mature in tissues

list the first step of inflammation after tissue/cell has been damaged
- damaged tissue and/or cell mediated histamine release
- vasodilation and leaky capillaries
which granulocyte is this:
- least common
- circulate in bloodstream
- allergic and helminth responses
- release histamine and heparin
basophils
basophils secrete what two compounds that result in reduction of clotting and increased blood flow
- histamine
- heparin
which granulocyte is this
- present primarily in GI and respiratory tract
- release oxygen radicals to kill microbes
- active in allergic rxns and asthma
- stimulate T-lymphocytes
eosinophils
eosinophils release what compound that causes airway smooth muscle contraction
leukotrienes
which of the granylocytes is weakly phagocytic
eosinophils
which of the granulocytes is particularly active against bacteria
neutrophils
which of the granulocytes is known as “first responder”
neutrophils
which granulocyte is this
- most abundant of the granulocytes
- circulate in bloodstream
- first responder
- release cytokines to amplify immune response
neutrophils