Lower GI Developmental Pathology Flashcards
(26 cards)
Which of the pictured anomalies of the trachea and esophagus is most common?

(Far left - 85%)
What is the VACTERL complex?
Association of several major classes of congenital anomalies
- Vertebral
- Anorectal
- Cardiac
- TEF
- Renal
- Limb
What prenatal and neonatal findings are consistent with TEF?
- Polyhydramnios
- Small stomach
- Prominent proxinal pouch
- Abnormal swallowing
- VACTERL association
- Excessive salivaiton, mucous
- Feeding intolerance
- Failure to pass NG/OG
Physiologic jaundice is a common finding in neonates. What (3) factor contribute to neonatal physiologic jaundice.
When should bilirubin begin to decrease in the infant?
Under what conditions should an infant be evaluated for abnormal jaundice (non-physiologic)?
Physiologic Jaundice
- Decreased RBC half-life compared to adults
- Immature liver has decreased capacity to conjugate/excrete bilirubin
- Decreased enterohepatic circulation
Bilirubin levels should begin to decline around Day 6-7
Abnormal jaundice:
- Jaundice beyond 2-3 weeks of age
- Direct bilirubin >2mg/dL
- Total bilirubin >12mg/dL in a term infant
- Total bilirubin >14mg/dL in a pre-term infant
When does neonatal biliary atresia typically present? Name some key findings.
Typical presentation: 4-6 weeks
Findings:
- Conjugated hyperbilirubinemia
- Acholic (light) stool, dark urine (coca-cola urine)
- Ultrasound abnormalities (gallbladder, spleen, situs inversus, etc)
- Abnormal IDA scan
- r/o other pathologies
Children with congenital biliary atresia typically require liver transplant or portoenterostomy by what age?
2 y.o. (death otherwise)
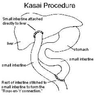
Describe the Kasai Procedure
Aproximately how many children achieve good long-term results?
Kasai Procedure
- Expose porta hepatis
- Transect small intestine (proximal jejunum?)
- Suture distal free end to porta hepatis
- Suture proximal free end to section of small bowel distally to porta hepatis
1/3 have good long-term results (especially if treated before 90 days old to avoid onset of bridging fibrosis)
Describe (3) important elements of postoperative care following the Kasai procedure for biliary atresia
- Supplement fat-soluble vitamins (ADEK) and monitor levels
- UDCA 20mg/kg per day for 2 years
- Ampicillin prophylaxis for chalangitis
What are the two most common types of choledochal cyst? Are they intra-hepatic or extra-hepatic?
What is the treatment commonly used for these two types?
Type I (77-90%) and Type IV (15%)
Both are extra-hepatic
Treatment: Excision with hepatico-jejunostomy or duodenostomy (with or without liver resection)
Give (4) processes that are pathogenic for congenital choledochal cysts
- Disordered organogenesis
- Pancreaticobiliary malunion
- Acquired weakness
- Distal obstruction
What type of anatomic variation of the pancreatic-biliary tree predisposes children to congenital coledochal cysts? Why?
Long common channel (>2cm)
The long common channel likely increases incidence of reflux of pancreatic enzymes into the bile ducts, causing irritation and cyst formation
What cancer is a common late complication of congenital coledochal cysts?
Biliary adenocarcinoma
Bilious emesis (any shade of yellow or green) in an infant… how bad?
SURGICAL EMERGENCY
What are Ladd’s Bands? How are these relevant to congenital malrotation of the gut?
What is Ladd’s procedure?
Ladd’s Bands: stalks of peritoneal tissue that attach the cecum to the abdominal wall. In malrotation, they may cross the duodenum and contribute to obstruction.
Ladd’s Procedure
- Untwist bowel
- Take down Ladd’s bands
- Widen mesentary (by cutting)
- Place small bowel on the right side, colon on the left side
- Perform appendectomy (so a future ER physician is not fooled by appendicitis symptoms presenting on the left side)
The Ligament of Treitz should always be *where* relative to the patient’s spine? What if it’s not?
Should be to the LEFT of the spine
If not, then suspect malrotation
The “Double bubble sign” is associated with what congenital malformation of the gut?
Duodenal atresia (failure of the duodenum to re-canalize around weeks 8-10)
What chromosomal defect is closely associated with duodenal atresia?
Where is the obstruction usually located?
How is this condition managed?
Trisomy 21 (Down Syndrome)
80% of obstructions are post-biliary (bilious emesis)
Surgical repair (duodenodueodenostomy)
What is the pathogenesis of jejunoileal atresia?
What type of inherited condition might contribute to the development of this disease?
What about external influences?
Is this condition commonly assocaited with extraintestinal problems (i.e. VACTERL or similar)?
What is the treatment?
In-utero vascular distruption leads to ischemic necrosis and resoprtion of a section of the developing bowel. This often leaves a gap or obstruction in the bowel (also a gap in the mesentery)
Inherited thrombophilia may contribute
Maternal use of vasoactive substances (pseudoephedrine, cocaine, nicotine)
Not commonly associated with extraintestinal anomalies
Treatment: surgery
What is Meckel’s Diverticulum?
How does it occur?
What are “the rules of 2”?
An outpouching of the small bowel that contains all four layers of the bowel: mucosa, submucosa, muscularis propria, and serosa
Results from the vitelline duct not involuting completely during development
- Occurs in 2% of population
- 2 types of abnormal lining (stomach and pancreas)
- Located within 2 feet of the ileocecal
- Usually 2 inches in length
- Usually symptomatic by age 2
How does Meckel’s Diverticulum present?
How is Meckel’s Diverticulum treated?
What does it look like on histology?
- bleeding into the intestine
- intestinal blcokage
- inflammation
Treated by surgical resection and reconnecting the healthy bowel
All four layers will be present, but gastric, pancreatic, and small bowel tissue may be side by side
What is Hirschprung’s disease?
What is the genetic mutation that causes it?
What genetic mutation is commonly associated with Hirschprung’s disease?
A lack of innervation in the bowel that causes obstruction
RET tyrosine kinase receptors (induce growth and differentiation in neural crest cells)
Trisomy 21 (AKA Down’s syndrome)
How is Hirschprung’s cured?
What negative results are seen on histology?
What positive results are seen on histology?
Resection and reattachment of non-innervated bowel
No Ganglion cells
Hypertrophic nerves are seen
What is necrotizing enterocolitis?
Who does it affect?
What causes it?
Widespread bowel death resulting in sepsis
mostly premature infants born <34 weeks
No one really knows; prematurity, formula feeding and dysbiosis are believed to contribute, but the cause is unknown
How does necrotizing enterocolitis present?
How is it diagnosed?
How is it treated?
Present with:
- Abdominal distension
- Feeding intolerance/emesis
- Rectal bleeding
- Temperature
- Abdominal wall erythema
Diagnosed by pneumatosis (air outline) on x-ray
Treated with:
- Stop feeding
- Broad spec IV antibiotics
- Transfusion/Mechanical Ventilation
- Peritoneal drainage or surgical resection


