Reproduction Lecture - Female Applied Anatomy Flashcards
(40 cards)
What are the 2 parts the uterus can be divided into?
- Body of uterus superior (2/3)
- Fundus
- Isthmus
- Uterine horns
- Cervix lower (1/3)
What are the 3 parts of the body of uterus?
- Fundus
- Isthmus
- Uterine horns
What can the cervix be divided into, and by what?
- Divided by the vaginal attachment into
- Supra-vaginal part
- Vaginal part
Where is the supra-vaginal part of cervix between?
- Between isthmus and vagina
What is the supra-vaginal part of uterus seperate from bladder and rectum by?
- Only separated from bladder anteriorly by loose connective tissue and from rectum posterior by recto-uterine pouch (pouch of Douglas)
What is the recto-uterine pouch also called?
Pouch of Douglas
What are the following relationships to the supra-vaginal part of cervix:
- anterior
- posterior
- lateral
- Anteriorly – urinary bladder
- Posteriorly – forms anterior wall of Douglas pouch
- Laterally – uterine artery (ureter below the uterine artery)
What part of the cervix is visible during speculum examination?
Vaginal part of cervix
What are the following arteries branches of:
- uterine artery
- vaginal artery
Both from anterior division of internal iliac artery
For the ovarian artery:
- origin
- enlosed within
- Origin
- Aorta
- Enclosed in
- The infundibulo-pelvis ligament
What does the ovarian vein anastomose with?
- Left
- Left renal vein
- Right
- IVC
What is the lymphatic drainage of:
- uterus
- ovaries
- Uterus
- Along uterine vessels within transverse cervical ligament to internal and external iliac lymph nodes and along uterosacral to sacral lymph nodes
- Ovaries
- Along ovarian vessels to the para-aortic lymph nodes
What are the 3 important nerves for the innervation of the female reproductive tract?
- Superior hypogastric plexus
- Inferior hypogastric plexus
- Pelvic splanchnic nerves
For superior hypogastric plexus:
- course
- contains
- division
- Course – in front of sacral promontory
- Contains – sympathetic nerve fibres
- Division – divides into right and left hypogastric nerves
For inferior hypogastric plexus:
- formed from
- course
- contains
- Formed from right and left hypogastric nerves and preganglionic parasympathetic fibres from pelvic splanchnic nerves
- Course – each side of rectum and base of bladder
- Contains – sympathetic and parasympathetic fibres
For pelvic splanchnic nerves:
- origin
- course
- contains
- Origin – S2/3/4
- Course – join hypogastric nerves to form inferior hypogastric plexuses
- Contains – pre-ganglionic para-sympathetic fibres
What are the functions of sympathetic and parasympathetic nerves in the pelvis?
- Sympathetic
- Inhibits peristalsis
- Stimulates contraction of genital organs during orgasm
- Parasympathetic
- Increases peristalsis
- Contraction of the bladder and rectum for urination and defecation
What are the 3 true ligaments of the female pelvis?
- Transverse cervical ligament
- From cervix and lateral part of vagina to lateral wall of pelvis
- Uterosacral ligament
- Superior and posteriorly from the side of cervix to middle of sacrum
- Pubocervical ligament/fascia

What does transverse cervical ligament extend from?
- From cervix and lateral part of vagina to lateral wall of pelvis
What does uterosacral ligament extend from and to?
- Superior and posteriorly from the side of cervix to middle of sacrum
What is A?

Superficial transverse perineal
What is B?
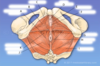
Deep transverse perineal
What is C?

Ischiocavernosus
What is D?

External urethral sphincter












