Thyroid Flashcards
(126 cards)
retinoid X receptor
thyroid hormone receptor

Activation of the THR (receptor)’s activity requires:
1) dimerization with the retinoid X receptor (RXR).
2) They bind to the Thyroid response element (TRE)
3) Stimulation or inhibition of a whole variety of genes
lab findings in grave’s disease
low serum TSH
high T4
use radioactive iodine to determine etiology (diffusely increseed in graves)
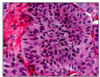
graves disease
obviously hyperfunctioning gland, hyperplasia, and hypertrophy of follicular cells.ar cells
follicular carcinoma
2nd ost common form of thyroid ca
slowly enlarging painless nodule
more common in areas w iodine deficiency
range from encapsulated to widely invasive tumors with necrosis and hemorrhgage
lower survival (age, size, invasion, metastasis)
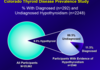
prevalence of hypothyroid
10% gen population
hashimoto’s thyroiditis pathogensesis
CD8+ cytotoxic t cell mediated cell death
ck mediated cell death (Th1)
binding of anti-thyroid abs

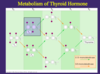
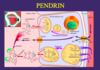
MIT
in colloid, when 1 iodine bound to a tyrosine ring
MIT + DIT = T3
if not made into TH, recycle iodine and tyrosine

follicular carcinoma
genetic mutations in papillary carcinoma
activation of MAP kinase pway - RET and BRAF
NOT seen in follicular adenoma/carcinoma - diagonsis!
RET/PTC rearrangements and BRAF point mutations are more or less specific for papillary carcinoma. Usually they’re not seen in follicular adenoma or carcinoma.
This is important because we use diagnostically and it is something I expect you to know.
subacute thyrodiitis
painful thyroiditis
due to release of pre-formed thyroid hormone (low radioactive iodine uptake)
may be associated with infections
parafollicular cells
C cells
1)deal with calcitonin hormone (calcium metabolism)
regulation of synthesis and secretion of TH
- availability of iodide
- stimulation by TSH
What is the most common subtype of graves disease?
thyroid stimulating immunoglobulin (TSI)
binds to the TSH receptor and mimics its actions stimulating the gland to release thyroid hormone
genetic mutations in graves
CTLA4
PTPN22
HLA-DR3
biochemical makeup of reverse T3
Reverse T3: inactive b/c you remove one inner iodine

Type I Deiodinase
5’ and 5
generate T3, Inactive T4 and T3
- Type 1 (mixed activator or inactivator) can take off 5 (inner ring) or 5’ (outer ring): present in liver, kidney, thyroid, and brain
- If 5’ à generates T3 active hormone
- If 5 (inner) à generates rT3 (inactive)

basic structure of thyroglobulin
lots of tyrosine!
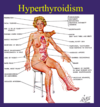
Mild hyperthryodiism
still dangerous
risk of a fib, tachycardia, APBs, reduced bone density
esp in elderly
Standard treatment for hypothyroidism
L Thyroxine (narrow TI, diff bioavailabilities)
May need to add Liothyronine (T3) - if deoidinase enzyme type 1 deficiency (rare)
Armour thyroid (natural products from animal thyroid - diff doses
iodine deficiency
endemic goiter with hypothyroidism
most common in areas away from sea water
available through certain foods, with supplments

hashimoto
diffusely enlarged gland: pale, nodular, rubbery
you would see diffusely enlarged thyroid gland which is pale and nodular because of the inflammation, fibrosis, and lymphocyte accumulation.

undifferentiated carcioma
Undifferentiated carcinoma is a very aggressive tumor that presents as a rapidly enlarging mass. It is seen in older patients. Mean survival is 6 months.
It just is a very ugly tumor and a very aggressive disease.
Which papillary carcinoma mutation is associated with papillary carcinoma most?
RET/PTC rearrangement

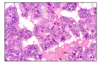
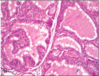
goiter - variably sized follicles some distended with colloid
Histologically you see variably sizes of thyroid follicles. Some of them are very big, some of them are ruptured, the colloid is in the stroma. Small ones. Then you see fibrosis.