Urticaria and Drug Rashes - Schwarzenberger Flashcards
(51 cards)
Describe the pathophysiology of urticaria
An inflammatory skin reaction caused by the release of histamine/other cytokines
Are all cases of urticaria allergen associated?
No, allergic or non-allergic
Timeframe of urticaria? Why is this important?
Each individual urticaria wheal will last no longer than 24 hours; if a single wheal lasts longer, reconsider the dx
(but whole episode can last longer)
What is angioedema in the context of urticaria? how long does it last?
swelling of the deeper dermis and subQ tissue; up to 72 hours
Drugs that commonly cause acute urticaria?
B-lactam abx, NSAIDs, ASA, opiates, IV radiocontrast
What cause of acute urticaria is seen in children frequently, but not in adults?
Food allergen induced
Differentiation between acute urticaria vs. chronic urticaria (how long does each last?)
Acute–> less than 6 weeks Chronic–> more than 6 weeks
Disease associated with chronic urticaria (I know it’s vague, she threw this out in class though)
Hashimoto’s Thyroiditis
Common locations of angioedema?
Lips, periorbital areas, hands, and feet
Why can ACE inhibitors cause angioedema?
Angiotensin converting enzyme normally breaks down Bradykinin
Hereditary angioedema cause (Angelina Jolie syndrome)?
(Angiolina Joliedema)
C1 inhibitor deficiency
Hoarseness in a patient in with angioedema. What are you worried about?
airway compromise
What is dermatographism?
condition of mast cell degranulation upon pressure application
What non immunologic things can cause urticaria?
Cold, heat, pressure, solar exposure, water
Primary therapy in uritcaria?
2nd generation anti-histamines
Why do you NOT use systemic glucocorticoids in urticaria?
risk of rebound urticaria
What is the most common cause of acute urticaria (hint: it’s not drug related)?
Viral infection
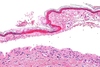
What do you assume as diagnosis when you see urticaria +24 hours (INDIVIDUAL lesions past 24 hours) ? What must you do at this point?
Assume urticarial vasculitis; biopsy the lesion
Risk factors for developing a cutaneous Rx rash?
Increased age, female gender, concomitant viral infection (HIV/EBV)
Most common drugs that cause cutaneous Rx induced rash (there’s 3)?
Abx, anticonvulsants, NSAIDs
Misdiagnose a patient with a bacterial infection and give them an abx. They break out with acute urticaria. What do you assume the correct diagnosis to be?
EBV infection; this precipitated the cutaneous abx rash
List the 5 types of cutaneous drug reactions discussed in the lecture? Frequency of 2 she mentioned?
- Morbilliform “maculopapular” rash - 90%
- Urticarial rash - 5%
- DRESS (Drug rash w/ eosinophilia and systemic symptoms
- Fixed Drug reaction
- Stevens-Johnson Syndrome/Toxic epidermal necrolysis
Most common distribution of cutaneous Rx rash?
90% are morbilliform (maculopapular)
Describe a mobilliform rash
Multiple small, pink, itchy papules on the trunk or pressure bearing areas (especially back/shoulders); spreads out over time to become confluent