Week 2 Flashcards
(175 cards)
Three general layers of vessels
Tunica intima
Tunica medical
Tunica adventitia

Endothelium
What types of epithelium is it? Exception?
What is the function of endothelium?
What signalling molecules does it secrete?
What is stored in endothelium (in arterioles and larger vessels)?
Enzymes?
Simple squamous (exception **cuboidal **in high venous endothelium in lymph node)
Smooth surface (promote flow/prevent clothing), Trasnport (H2O, electrolytes, O2, CO2)
NO (vasodilation), Endothelin (vasoconstrictor), Collagen and laminin (extra cellular matrix)
Wiebel-Palade bodies store vWF
Angiotensin-converting enzyme (ACE) AI→ AII
Inactivate bradykinin, serotonin, prostaglandin
Basal lamina of endothelial cells
What is it between?
Endothelium and Subendothelial tissue

What is the subendothelial connective tissue made of?
Loose CT with scattered smooth muscle cells
Internal elastic fiber?
What is it made of and in what arrangement?
What may pass through internal elastic fibers? Purpose?
Fenestrated sheet of elastin
Processes of endothelial cells (to form gap junctions with smooth muscle in tunica media)
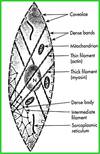
Cell layers from inside of the blood vessel to outside
Which layer TI/TM/TA do they belong to?
Endothelium (TI)
Basal lamina (TI)
Subendothelial connective tissue (TI)
Internal elastic membrane (TI)
Smooth muscle (TM)
External elastic membrane (TM)
Adventitia (TA)
Tunica media
Composition?
Large vessels vs. small vessels?
Where this layer is not present?
Smooth muscle, elastin, collagen (varies)
Small vessels: pericytes (contractile)
Large vessels: external elastic laima
Capillaries / post capillary venules

Tunica adventitia
Composition?
Unique structures?
Fibroblasts, collagen, elastic fibers
Vasa vasorum, nerves
Where are the post-synaptic nerves?
How do they reach smooth muscle?
When stimulated by sympathetic which vessels dilate and which contract?
Tunica adventitia
Release norepinephrine and it diffusses through EEL. Propagation through gap junction.
Vessels assocaited with skeletal muscle dilate, and all others contract
Blood supply to blood vessels
Small vessels vs. large vessels?
In which blood vessels the blood supply to blood vessels more prevalent? Why?
Vasa vasorum supplies the elastic and muscular arteries.
Small vessels receive O2 by diffusion, while large vessels have capillary beds in tunica media
Veins, less oxygen
Three types of artiers?
Elastic, Muscular, and Arteriole

Elastic artery
Location of these arteries?
Prominent structure in tunica media? Function?
Prominent structure in tunica adventitia? Function?
Conduction of blood from heart
40-70 fenestrated layers of elastin alternating with smooth muscle – allow to strech and recoil
Loose fibroelastic tissue allows movement and distention

Muscular artery
Location of these arteries?
What structures are prominent about layers?
Vasa vasorum?
Distributing arteries (most named down to 0.1 mm)
Internal elastic lamina (with endothelium / gap junctions)
Thick tunica media with smooth muscle. Gap junctions connect all layers of smooth muscle.
Extenal elastic lamina (fenestrated for neutrotransmitters from unmyelinated neurons)
Vasa vasorum less prominent

Arteriole
Layers?
Which layers cannot be distinguished?
Tunica intima and media
Adventitia cannot be distinguished from CT

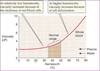
Corresponding Arteries vs. Veins
Size?
Tunica media?
Shape?
Where blood cells are usually not found?
Size: Veins > Arteries
Tunica media: Arteries > Veins
Shape: Arteries circular
Where blood cells are usually not found: arteries
Luminal diameter defintion
Width of arteriole wall approx
Capillaries
Size?
Tunica media / adventitia?
Function?
Three types?
8-10 uM (diameter of single RBC)
No
Provide oxygen and control temperature
Continuous, fenestrated, sinusoidal

Capillaries types characterstiics
Location?
Characteristic?
Location:
Continuous: nervous (modified in brain to limit passage), muscle, and connective tissue
Fenestrated: pancreas, renal glomerulus (without diaphgram)
Sinusoidal: Spleen, liver, bone marrow of lymphoid organs
Layer charactersitics:
Continuous: Diaphram with endothelial cells with tight junctions
Fenestrated: Diiaphagram covering pores (
Sinusoidal: Discontinuous endothelial wall with basal lamina forming irregular channels

Are veins or arteries more numerous?
Which one is more permeable? Importance?
Veins
Veins (high endothelial venules)
Veins
Characteristic of large veins?
Sizes?
Characteristics of pulmonary/leg veins?
Charactersitic structure of veins?
More developed tunica adventitia than tunica media
venules >20um, medium vein >1cm, sm >1mm
Veins in legs/pulmonary system have smooth muscle
Valves (extensions of tunica intima)

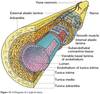
Three heart layers
Component of endocadrium?
Subendocardial layer?
Myocardial cells function?
What is another name for epicardium?
What travels through epicardium?
Endocardium, Myocardium, Epicardium
Endothelial cells (continuous with vessels), CT, smooth muscle cells
Suendocardial contain CT, nerves, blood vessels, purkinje fibers
Attach to fibrous skeleton, contraction, secrete hormones
Visceral layer of pericardium
Coronary arteries
Where does the signal travel from AV?
AV node
bundle of His
bundle branches
Purkinje fibers
Lymphatic System
How does it differ from cardiovascular?
Strcuture of the wall?
Layers?
No pump, one way flow (to heart)
Endothelial cells anchored by fillaments
In ducts, there are three similar layers to blood vessels
Shortness of breath when lying flat (manifestation of heart failure)
Orthopnea