Regulation of Arteriolar resistance Flashcards
What is Darcy’s law?
Flow = ?

What does poiselluille’s law tell us about resistance?
Resistance of a vessel is mainly determined by the radius of the vessel
If flow = difference in pressure / resistance what does pressure equal?
Flow x resistance
How can you denote darcy’s law in terms of systemic circulation?
Flow = difference in pressure /resistance
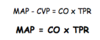
CO = Mean arterial pressure / total peripheral resistance : therefore
Mean arterial pressure = CO x total peripheral resistance
What does arteriolar radius affect?
Flow through individular vascular beds
AND
Mean arterial pressure
What is done to keep blood flow to each vascular bed sufficient as well as keeping mean arterial pressure in the right range?
Resistance juggling
Two levels of control over the smooth muscle surrounding arterioles:
- Intrinsic mechanisms - concerned with meeting the selfish needs of each individual tissue
- Extrinsic mechanisms - concerned with ensuring that the total peripheral resistance of the whole body stays in the right ball park
What controls extrinsic control?
Nerves and hormones
What is the neural extrinsic control?
- Sympathetic nerves
- release noradrenaline
- binds to a1-receptors
- causes arteriolar constriction
- therefore decreased flow through that tissue, and tends to increase TPR
- Parasympathetic nerves
- usually no effect
What is the hormonal extrinsic control?
•noradrenaline
–released from adrenal medulla
–binds to a1-receptors
–causes arteriolar constriction
–therefore decreased flow through that tissue, and tends to increase TPR
BUT in some tissues, eg skeletal and cardiac muscle, it also activates b2-receptors
- causes arteriolar dilation
- therefore increase flow through that tissue, and tends to decreaseTPR
Name the other hormonal extrinsic control mechanisms
Angiotensin - When blood volume is LOW - causes arteriolar constriction
Vasopressin - (antidiuretic hormone) - When blood volume is LOW - causes arteriolar constriction
Atrial natriuretic peptide & Brain natriuretic peptide - When blood volume is HIGH - causes arteriolar dilation.
How do ACE inhibitors work?
ACE inhibitors are used to decrease blood pressure
ACE is angiotensin converting enzyme (converts angiotensin 1 to angiotensin 2)
ACE inhibitor reduces the amount of angiotensin 2 and so decreases total peripheral resistance
What are the intrinsic methods of control of arteriolar resistance?
Active (metabolic hyperaemia)
Pressure (flow) autoregulation
Reactive hyperaemia
The injury response
What is meant by hyperaemia?
Hyperaemia is an increase in blood flow due to an increase in metabolism
How does active hyperaemia result in arteriole dilation?
Increase in metabolic activity - increase concentraion of metabolites
Triggers the release of EDFR (Endothelium derived relaxing factor- paracrin/local effect)
Increase flow to wash out metabolites
Blood supply matches metabolic needs

How does pressure autoregulation result in arterile dilation?
Decrease mean arterial pressure - reduced flow
Metabolites accumulate
EDFR

