Week 5: Toxin-mediated infections Flashcards
What is a bacterial toxin?
PRotein or lipopolysaccharide toxin secreted by or remaining a component of the bacteria
What is an exotoxin?
Toxin secreted by bacteria
What is an endotoxin?
Toxin that remains a component of bacteria (eg in the cell membrane)
Examples of exotoxins
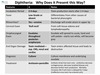
- Diptheria toxin
- Pertussis toxin
- Shiga toxin
- Botulinum toxin
- Tetanus toxin
Examples of endotoxins
- LPS in gram negative bacteria
- Normally lipopolysaccharide complexes
Tropism of toxins
eg
- neurotoxin indicates nervous system
- enterotoxin indicates GI tract
Protein toxin components
- protein toxins often have 2 components (A and B units)
- one bind to a receptor and another with enzymatic capabilities
Examples of toxins involved in invasive infections
- Spe B in necrotizing fasciitis
Toxins that commonly cause problems from a distance WITHOUT invasion
- Botulism
- Tetanus
Question
What is the most potent toxin?
A. Strychine
B. Rattlesnake Venom
C. Botulinum toxin
D. Tetanus toxin

C. Botulinum toxin
Relative toxin potencies

Clinical case

Necrotizing Fascitis (often associated following varicella)

Toxin mediated disease NOT associated with a single organism
Necrotizing fasciitis
How does necrotizing fasciitis present?
- Rapid spread (hours)
- Initially pain is out of proportion
- Appear sicker than one might expect
- As disease progresses pain lessens (nerves destroyed)
- Progressively worse local perfusion (capillaries destroyed)
- ‘Brawny’ edema of the affected site (feels like wrestling mat on skin)
- Frequent sepsis/hypotension
Toxins with a potential role in Necrotizing Fasciitis
- Leukocidin
- Exfoliatin B
- Streptolysin O
- Streptococcal pyrogenic exotoxin E
- Streptococcal pyrogenic exotocin B
Organisms that produce toxins in necrotizing fasciitis
- S. aureus
- S. pyogenes
Toxins produced by S. aureus in necrotizing fasciitis
- Leukocidin
- Exfoliatin B
Toxins produced by S. pyogenes in necrotizing fasciitis
- Streptolysin O
- Streptococcal pyrogenic exotoxin E
- Streptococcal pyrogenic exotoxin B
Leukocydin is produced by?
S. aureus
Exfoliatin B is produced by?
S. aureus
Streptolysin O is produced by?
S. pyogenes
Streptococcal pyrogenic exotoxin E is produced by?
S. pyogenes
Streptococcal pyrogenic exotoxin B is produced by?
S. pyogenes
Leukocidin toxic effect
Destruction of phagocyte membranes
Exfoliatin B toxic effect
epidermal cleavage
Streptolysin O toxic effect
Destruction of cholesterol
Streptococcal pyrogenic exotoxin E toxic effect
Superantigen formation
Streptococcal pyrogenic exotoxin B toxic effect
Cysteine protease
Mortality rate of necrotizing fasciitis in adults
24%
Mortality rate of necrotizing fasciitis in pediatric
10%
Mortality rate of necrotizing fasciitis in neonates
50%
Necrotizing fasciitis how many organisms in adults?
most are polymicrobial infections
Necrotizing fasciitis how many organisms in pediatrics?
Most are monomicrobial Group A Strep
Necrotizing fasciitis is commonly associated with the development of?
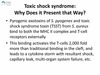
Toxic Shock Syndrome
Treatment of Necrotizing Fasciitis
- QUICK to surgery for debriding
- Also antibiotics

Question


Why does Necrotizing Fasciitis present the way it does?

The most important thing in treating Necortizing Fasciitis
Time to surgery (GET THERE QUICK)