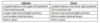
Anatomy Flashcards
(229 cards)
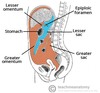
Where does the Upper GI tract end?
Duodenum
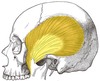
Which 3 pairs of muscles are responsible for closing the jaw?
Masseter, Temporalis and Medial pterygiod
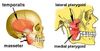
Which pair of muscles is responsible for opening the jaw?
Lateral pterygoid

What is the origin and insertion of the masseter m.?
Angle of mandible to zygomatic arch

What is the origin and insertion of the temporalis m.?
Coronoid process of mandible to temporal fossa
What is the origin and insertion of the medial pterygoid m.?
Angle of mandible (medial side) to pterygoid plates of sphenoid bone

What is the origin and insertion of the lateral pterygoid m.?
Condyle of mandible to pterygoid plates of sphenoid bone

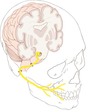
Which nerve supplies all of the muscles acting on the jaw?
Mandibular division of trigeminal nerve – CN V3

Which is the only nerve that attaches to the pons?
Trigeminal nerve
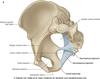
How does the V3 - mandibular branch of trigeminal nerve leave the skull?
Through the sphenoid bone at the foramen ovale

What sits in between the arches of the soft palate?
Palatine tonsils

Where does the anterior 2/3rds of the tongue reside and in what plane does it lie?
It is in the oral cavity, and lies horizontally
Which nerve provides the general sensory supply to the anterior 2/3rds of the tongue?
CN V3 - specifically the lingual nerve (branch of mandibular branch)

Which nerve provides the special sensory supply to the anterior 2/3rds of the tongue?
CN VII (facial)

Where does the posterior 1/3rd of the tongue reside and in what plane does it lie?
It is not in the oral cavity, it is technically the anterior wall of the oropharynx. It lies vertically
Which nerve provides the general and special sensory supply to the posterior 1/3rd of the tongue?
CN IX - Glossopharyngeal nerve

Which nerve supplies general sensation of the superior half of the oral cavity?
CN V2 - Maxillary branch of Trigeminal
Which nerve supplies general sensation of the inferior half of the oral cavity?
CN V3 - Mandibular branch of Trigeminal
What is the gag reflex?
A protective reflex that prevents foreign bodies from entering the pharynx or larynx. Part of the reflex response to touching the posterior wall of the oropharynx is to constrict the pharynx, as the patient attempts to close it off as an entry point into the body
Which nerve provides the sensory supply to the gag reflex?
CN IX - Glossopharyngeal n.
Which nerve provides the motor supply to the gag reflex?
CN IX and CN X - Glossopharyngeal and vagus n.
What is the purpose of spraying a local anaesthetic prior to a endoscopy?
‘block’ sensory action potentials in CN V2, V3, VII and IX, which supply the general sensation to the superior and inferior lower cavity, and sensory and motor supply of gag reflex, respectively
What is the intracranial course of the trigeminal nerve?
Leaves the pons, and passes inferior to the edge go the tentorium cerebella between the posterior and middle cranial fosse
How does V2 - maxillary branch of trigeminal leave the skull?
Through the sphenoid bona via the foramen rotundum