Liver Conditions Flashcards
(197 cards)
What duration defines chronic liver disease?
Disease greater than 6 months
What is the clinical pathway of cirrhosis?
1) Causes of chronic liver disease - presents as signs and symptoms of the causal disease
2) Recurrent inflammation and process of fibrosis
3) Compensated cirrhosis - presents with stigmata of cirrhosis
4) Decompensated cirrhosis leading to chronic liver failure or acute-on-chronic liver disease

What are the 4 cells of the liver?
Hepatocytes, Endothelial cells, Kupffer cells and Hepatic stellate cells
What is the function of hepatic stellate cells?
Storage of vitamin A as retinol
What is the function of Endothelial cells in the liver?
Regulate the passage of molecules from the blood to the liver
What is the function of Kupffer cells?
Liver’s own immune system
What is liver fibrosis?
The accumulation of tough, fibrous scar tissue in the liver as a result of injury healing process going wrong
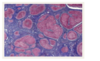
What is the pathophysiology of progression of fibrosis to cirrhosis?
1) Hepatocytes are injured due to infection with a virus, heavy alcohol consumption, toxins, trauma etc, and activates the immune system.
2) Hepatocyte injury stimulates inflammatory immune cells to release cytokines, growth factors etc which direct hepatic stellate cells (source of most ECM) to activate and produce collagen type I and III, glycoproteins, proteoglycans, and other substances
3) These substances are deposited in the hepatic parenchyma and space of disse of the liver, the latter causing capillarisation - where capillaries lose fenestration which blocks exchange (portal hypertension)
4) At the same time, the process of breaking down or degrading collagen is impaired so regeneration is limited to small nodules
What is Chronic Liver Disease, and what is it not?
Chronic liver disease is a disease process resulting in cirrhosis – not a disease in itself
How long does it normally take to get from a healthy liver to chronic liver disease?
20 years
What are the main causes of cirrhosis?
Common: - Alcohol - NAFLD - Hep C/B - PBC/PSC - Autoimmune hep Less common: -Haemachromotosis - Wilson’s -alpha 1 antitrypsin
What actually is cirrhosis?
Pathological end-stage of any chronic liver disease. Irreversible liver damage with loss of normal liver architecture histologically with bridging fibrosis and nodular regeneration
What is steatosis?
Infiltration of liver cells with fat, associated with disturbance of the metabolism by, for example, alcoholism, malnutrition, pregnancy, or drug therapy.
What is the most common cause of chronic liver disease in the western world?
NAFLD
What is the 2 Hit Paradigm for the pathophysiology of NAFLD?
First hit: Most likely insulin resistance leading to accumulation of triglycerides in the liver and hepatic steatosis development Second hit: additional oxidative injury required to manifest the nectro-inflammatory component
True or False: NAFLD and metabolic syndrome aren’t associated
False, nice try
What is the relationship between NASH and NAFLD?
NAFLD is an umbrella term which encompasses simple steatosis (fatty liver) without liver inflammation, and Non-alcohol steatohepatitis (NASH) where there is inflammation as a result of fatty infiltration with risk of fibrosis and cirrhosis
How would you differentiate between simple steatosis and NASH?
US and Liver biopsy
Which conditions does auto-immune liver disease cover?
• Primary Biliary Cholangitis (Cirrhosis) • Auto-immune Hepatitis • Primary Sclerosing Cholangitis
What is Primary Biliary Cholangitis?
Chronic autoimmune disease where the epithelial cells of the small intrahepatic bile ducts are damaged by the immune system. Characterised by progressive bile duct damage (and eventual fibrosis/loss)
What is the underlying aetiology of PBC?
There is a very high incidence of autoantibodies, most characteristically directed against mitochondrial antigens (antimitochondrial antibody).
What is the pathophysiology of PBC?
Process in PBC is damage to, and progressive destruction of, the biliary epithelial cells lining the small intrahepatic bile ducts. Bile ducts are damaged in the context of portal tract inflammation, further supporting the concept of an autoimmune component to the disease. Loss of bile duct cross-sectional area within the liver leads to cholestasis with progressive bile acid retention. Bile acid pooling can cause secondary damage within the liver, further contributing to progressive bile duct loss
Which is more common in women: PBC or PSC?
PBC (B for burds)
What are the symptoms of PBC?
Asymptomatic initially, then fatigue, itch without rash, xanthesalma and xanthomas