Bariatric Surgery Flashcards
(68 cards)
Indications for Bariatric surgery?3
- BMI ≥ 40 kg/m2 without comorbidities
- BMI 35-39.9 kg/m2 with comorbidity
- BMI 30-34.9 kg/m2 (w/specific comorbodities)
BMI 35-39.9 kg/m2 with comorbidity which comorbities? 13
- Type 2 DM 2. OSA
- HTN
- Hyperlipidemia
- Obesity-hypoventilation syndrome (OHS)
- Pickwickian syndrome (OSA+OHS)
- Nonalcoholic steatohepatitis (NASH)
- Pseudotumor cerebri
- GERD
- Venous stasis disease
- Severe urinary incontinence
- Debilitation arthritis
- Impaired quality of life
BMI 30-34.9 kg/m2 with what comorbidites? 2
- Uncontrollable Type 2 DM
- Metabolic syndrome Lack of evidence to support long term benefit in this group
Contraindications to bariatric surgery? 10
- History of bulimia
- Age > 65 or less than 18
- For lipid or glycemic control
- For CV risk reduction
- Untreated major depression or psychosis
- Binge-eating disorders
- Current drug or alcohol abuse
- Severe cardiac disease with prohibitive anesthetic risks
- Severe coagulopathy
- Inability to comply with requirements including (life-long nutritional supplements) & dietary changes**
Preoperative assessment includes what? 3
- Psychological
- Medical
- Anesthetic risk
Preoperative assessment requires a team approach Who? 5
- Nutritionist
- Medical bariatric specialist
- Psychologist/Psychiatrist
- Clinical nurse specialist
- Surgeon
Goals of the psychologic assessment 4
- Is the patient able and willing to make the necessary changes?
- Identification of mental disorders
- Social history in regards to previous weight loss attempts, physical activity, substance abuse, compulsive eating
- Does the patient have the cognitive ability to do this and the support to carry it through?
Components of the psychological assessment 4
- Behavioral
- Cognitive/emotional
- Current life situation
- Expectations
Medical assessment includes? 2
Complete history and physical exam
Mechanisms of weight loss with surgery 3
Restriction
Malabsorption
Both
Restrictive surgeries do what? What are the three general processes?
Limit caloric intake by reducing the stomach’s capacity:
- Resection
- Bypass
- Creation of a proximal gastric outlet
Specific Restrictive surgeries? 3
- Vertical banded gastroplasty
- Laparoscopic adjustable gastric banding
- Sleeve gastrectomy
Malabsorptive surgeries do what? How is this accomplished? 2
Decrease the effectiveness of nutrient absorption by shortening the length of the functional small intestine:
- bypass of the small bowel absorptive surface area
- diversion of the biliopancreatic secretions that facilitate absorption
Malabsorption surgeries 2
- Jejunoileal bypass
- Duodenal switch operation
Combination restrictive/malabsorptive surgeries 3
- Roux-en-Y gastric bypass (RYGB)
- Biliopancreatic diversion
- Biliopancreatic diversion with duodenal switch
3 Most common bariatric surgeries
- Roux-en-Y gastric bypass (47%)
- Sleeve gastrectomy (28%)
- Laparoscopic adjustable gastric band (18%)
Roux-en Y gastric bypass (RYGB)
Most commonly performed bariatric surgery in the US
47% of weight loss surgeries done in 2011
Describe this?

RYGB surgery
- Gastric pouch is how big?
- Gastric pouch attached to a section of small bowel ______cm in length (gastrojejunostomy)
- Cut ends of the _____________and the __________are then connected 75 to 150 cm distal from the gastrojejunostomy
- Gastric pouch less than 30 ml
- 75-150 cm in length (gastrojejunostomy)
- biliopancreatic limb, the Roux limb
RYGB
Major digestion and absorption of nutrients occurs where?
in the common channel where pancreatic enzymes and bile mix
Weight loss mechanism
- What part of restrictive?
- What contributes to the malabsorption part?
- What suppressses the appetite?
- What two substances are increased post bypass? and what will this promote?
- Small pouch is restrictive
- There is malabsorption because of the “removed” small bowel
- Ghrelin inhibition (suppresses appetite)
- GLP-1 and CCK increased post bypass (may promote an anorectic state)
Gastrojejunostomy can result in ____________with high sugar meals
Describe this?
- Dumping syndrome
- lightheadedness, nausea, diaphoresis and/or abdominal pain, and diarrhea
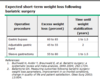
Expected weight loss with RYGB
Up to 70% of extra weight in 2 years
Describe the Sleeve gastrectomy?
Second most common weight loss surgery performed worldwide
28% of all procedures in 2011

Sleeve Gastrectomy
- Most of the what is removed?
- Advantages? 2
- New stomach is resistant to what?
- Contains a few _______producing cells
- Most of the greater curvature of the stomach is removed
- Safer and technically less difficult to perform than RYGB
- New stomach is resistant to stretching without the fundus
- ghrelin