Blood Gas Carriage Flashcards
(47 cards)
Is oxygen soluble in water?
Not very
How much dissolved oxygen does plasma contain at a partial pressure of 13.3kPa and a temperature of 37oC?
0.13mmol/L
How much oxygen do we need at rest?
12mmol per minute
What volume of plasma would be required to meet the bodys oxygen requirements if the only source was dissolved oxygen?
92L
What is the typical ppO2 in the lungs?
13.3kPa
What is the typical ppO2 in the tissues?
~5kPa
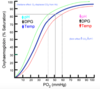
Draw an oxygen haemoglobin dissociation curve

What does haemoglobin do?
With respect to oxygen binding
Reversibly binds to oxygen over a very narrow range of ppO2
Describe the structure of haemoglobin
Tetrameric protein, made up of 2 α and 2 ß subunits, with 4 haem groups
What is the result of haemoglobin having 4 Haem groups?
It can bind to four molecules of oxygen
What factors can decrease the affinity of Hb for O2?
- H+
- Increasing temperature
- Increased CO2
What happens at sites of low pH and increased CO2?
More oxygen is required and will be released
What tissue may experience low pH and increased CO2?
Muscle tissue during exercise
What is the effect of low pH and increased CO2 on haemoglobin dissociation called?
The Bohr effect
What happens to the oxygen dissociation curve as a result of the Bohr effect?
It shifts to the right
Draw a graph illustrating the effect of changing conditions on the oxygen dissociation curve
What happens if the pO2 in the capillaries falls?
pH falls and temperature falls, so Hb will give up more oxygen
What is the result of a pO2 fall in the capillaries on the saturation of Hb leaving the capillaries?
It is greatly reduced
What can be used to calculated the percentage of oxygen that has been given up in a tissue if venous pO2 is known?
A dissociation curve
What happens to blood flowing through alveolar capillaries?
It picks up oxygen and looses carbon dioxide by diffusion of those gases across the alveolar wall
What is the rate at which gases exchange determined by?
- Area available for exchange
- Resistance to diffusion
- Gradient of partial pressure
What can be used to calculate the transfer factor of the lungs?
Carbon Monoxide
What reactions can carbon dioxide undertake in the blood?
- Dissolves in water
- Reacts in water
- Binds directly to proteins
How does the solubility of carbon dioxide compare to that of oxygen?
It is more soluble


