Lower GI pathology Flashcards
(60 cards)
What are the types of GI pathology?
Congenital
Acquired
Mechanical
Infection
Inflammation
Ischaemia
Tumour
What are the general symptoms of large bowel pathology?
Disturbance of normal function (diarrhoea, constipation)
Bleeding
Perforation/fistula formation
Obstruction
+/- Systemic illness
What are congenital GI disorders?
Atresia/stenosis
Duplication
Imperforate anus
What is Hirschsprung’s disease?
Absence of ganglion cells in myenteric plexus,
Distal colon fails to dilate
80% male
Constipation, abdominal distension, vomiting, ‘overflow’ diarrhoea
Associated with Down’s syndrome (2%)
RET proto-oncogene Cr10 + others
How do you diagnose Hirschsprungs disease?
clinical impression
biopsy of affected segment.
hypertrophied nerve fibers but no ganglia.
Treatment: resection of affected (constricted) segment. (frozen section)
What are mechanical bowel disorders?
Obstruction
Adhesions
Herniation
Extrinsic mass
Volvulus
Diverticular disease
What is a volvulus?
Complete twisting of a loop of bowel at mesenteric base, around vascular pedicle intestinal obstruction +/- infarction small bowel (infants) sigmoid colon (elderly)
What is the pathogenesis of diverticular disease?
High incidence in West
Low fibre diet
High intraluminal pressure
‘Weak points’ in wall of bowel
90% occur in left colon
What are the complications of diverticular disease?
Pain
Diverticulitis
Gross perforation
Fistula (bowel, bladder, vagina)
Obstruction
What are the inflammatory disorders of the large bowel?
Acute colitis
Infection (bacterial, viral, protozoal etc.)
Drug/toxin (esp.antibiotic)
Chemotherapy
Radiation
Chronic colitis
Crohn’s
Ulcerative colitis
TB
What are the infectious colitis’
Viral
Bacterial
Protozoal
Fungal
What are the effects of GI infection?
Secretory diarrhoea (toxin)
Exudative diarrhoea (invasion and mucosal damage)
Severe tissue damage + perforation
Systemic illness
(biopsy)
What is pseudomembranous colitis?
Antibiotic associated colitis
Acute colitis with pseudomembrane formation
Caused by protein exotoxins of C.difficile
How do you diagnose pseudomembranous colitis?
Histology: Characteristic microscopic features on biopsy
Laboratory: C. difficile toxin stool assay
Therapy: Metronidazole or Vancomycin
What is ischaemic bowel?
Acute or chronic
Most common vascular disorder of the intestinal tract
Usually occurs in segments in “watershed” zones, e.g. splenic flexure (SMA and IMA) and the rectosigmoid (IMA and internal iliac artery)
Mucosal, mural, transmural (perforation)
What is the aetiology of ischaemic colitis?
Arterial Occlusion: atheroma, thrombosis, embolism
Venous Occlusion: thrombus, hypercoagulable states
Small Vessel Disease: DM, cholesterol emboli, vasculitis
Low Flow States: CCF, haemorrhage, shock
Obstruction: hernia, intussusception, volvulus, adhesions
What is IBD?
Crohn’s disease or Ulcerative colitis
Diagnosis of exclusion
What is the aetiology of IBD?
?Genetic predisposition (familial aggregation, twin studies, HLA )
?Infection (Mycobacteria, Measles etc)
?Abnormal host immunoreactivity
->Inflammation
What are the clinical features of IBD?
Diarrhoea +/- blood
Fever
Abdominal pain
Acute abdomen
Anaemia
Weight loss
Extra-intestinal manifestations
Who gets Crohn’s?
Western populations
Occurs at any age but peak onset in teens/twenties
White 2-5x > non-white
Higher incidence in Jewish population
Smoking
Where is affected in Crohn’s?
Whole of GI tract can be affected (mouth to anus)
‘Skip lesions’
Transmural inflammation
Non-caseating granulomas
Sinus/fistula formation
‘Fat wrapping’
Thick ‘rubber-hose’ like wall
Narrow lumen
‘cobblestone mucosa’
Linear ulcers
Fissures
abscesses
What are the extra intestinal manifestations of Crohns?
Arthritis
Uveitis
Stomatitis/cheilitis
Skin lesions
Pyoderma gangrenosum
Erythema multiforme
Erythema nodosum
Who gets UC?
Slightly more common than Crohn’s
Whites > non-whites
Peak 20-25 years but can affect any age
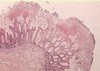
What does UC cause?
Involves rectum and colon in contiguous fashion.
May see mild ‘backwash ileitis’ and appendiceal involvement but small bowel and proximal GI tract not affected.
Inflammation confined to mucosa
Bowel wall normal thickness
Shallow ulcers