Penile and Testicular Carcinoma Flashcards
(61 cards)
where is penile cancer most common
rare in the UK, more common in the far east and africa (poor hygiene)
is penile cancer more common in circumcised or uncircumcised individuals
rare in circumcised individuals
phimosis
- inability to retract the foreskin
- associated with BXO
name 2 pre malignant cutaenous penile lesions
- BXO
- leukoplakia
BXO
- white patches, fissuring, bleeding and scarring that usually affects the tip of the glans
- the urethra may narrow, resulting in poor urine flow and requiring dilatation
- can cause phimosis

how is BXO treated
circumcision and glans resurfacing
leukoplakia in the penis
- pre malignant lesion
- abnormal white spots that may form around the urethra opening

what is the peak age for penile SCC
80
causes of penile SCC
- poor hygiene
- there is an association with HPV 16
name 2 forms of penile SCC in situ
- Bowen’s
- erythroplasia of queyrat
Bowen’s disease
- CIS
- red patches on the genitalia

erythroplasia of queyrat
- CIS
- a form of Bowen’s disease
- occurs on the glans, prepuce or shaft of penis
what are Bowen’s disease and EoQ precursors for and associated with
precursors for invasive SCC and associated with HPV 16
which tumours can be managed with circumcision
those on the prepuce
treatment for penile CIS
topical 5 fluourouracil (cytotoxic)
when does most invasive SCC present
delayed - most have already spread to a lymph node
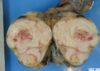
presentation of invasive penile SCC
- red area/mass/nodule on the penis
- can ulcerate
- phimosis
- itching, fungating mass
- foul smell
- advanced cases may cause haematuria

investigation of a primary penile tumour
- physical examination
- cytological and histological diagnosis
- US
- MRI if US inconclusive
investigation of lymph nodes
radonuclide sentinel node biopsy
investigation of metastases
CT, bone scan in symptomatic patients
where does lymph from the penis, testis and scrotum drain
- Lymph from the scrotum & most of the penis (not the glans) drains to the superficial inguinal lymph nodes found in the superficial fascia in the groin
- Lymph from the testis drains to the lumbar nodes around the abdominal aorta

outline the arterial blood supply to the penis and scrotum
- Blood supply to the penis is via the deep arteries of the penis; branches of the internal pudendal artery (from the internal iliac)
- Blood supply to the scrotum is via the internal pudendal and branches from the external iliac artery

staging of penile invasive SCC
TNM

management of invasive penile SCC
total or partial penectomy and reconstruction