Radiotherapy and Chemotherapy in Gynaecological Cancers 1 Flashcards
(27 cards)
Occurrence of ovarian cancer?
Tends to occur in women aged >50 years
It is more common in women with:
- Nulliparity
- Delayed pregnancy
- FH of breast or ovarian cancer (most cases are sporadic though); offer referral to clinical genetics
Genetic mutations that predispose to ovarian cancer?
BRCA1 (40% risk)
BRCA 2 (18% risk)
HNPCC (Lynch syndrome)
Presentation of ovarian cancer?
Often presents late, with non-specific symptoms:
- Ascites / bloating
- Pelvic mass / bladder dysfunction
- Pleural effusion / SoB
NOTE - it is often misdiagnosed as IBS
It can be an incidental finding
When should a diagnosis of ovarian cancer be considered?
In women presenting with 1 or more symptoms; the main symptom is abdominal distension with or without bloating, with additional symptoms of:
- Abdominal/pelvic pain
- Feeling full quickly (early satiety)
- Difficulty eating (loss of appetite)
- Urinary symptoms (urge, frequency, etc)
If these are of <12 months duration and occurring >12 times per month, consider ovarian cancer; esp. suspicious if patient is >50 years of age
Initial Ix for ovarian cancer?
CA 125 (tumour marker) blood serum level
Urgent pelvic USS carried out in women with persistent abdominal distension, early satiety, loss of appetite, pelvic/abdominal pain, increase
If symptoms persist or worsen, despite a normal CA 125 and a -ve USS, refer to secondary care
Acronym for ovarian cancer signs?
BEAT
B - bloating that is persistent and does not come & go
E - eating less and feeling fuller
A - abdominal and pelvic pain that is persistent
T- tell your GP
NOTE - may also have increased abdominal size
Use of screening for ovarian cancer in the general population?
Should not be performed outwith the research setting, as it has been shown to confer not benefit in saving lives
Which women should be offered genetic risk assessment?
All women with non-mucinous ovarian or fallopian tube cancers (for BRCA1 and 2)
Women with ovarian cancer who have an FH of breast, ovarian or colon cancer
Consider BRCA1 and 2 mutation analysis in a family where there is a ≥10% risk of a mutation being present
Management of women with BRCA or BRCA2 gene mutations?
Offer prophylactic salpingo-oophorectomy at a relevant time in their life
After oophorectomy, hormone replacement can be used until the time of natural menopause, without losing the benefits of breast cancer risk reduction
Ix used to diagnose ovarian cancer?
Blood test is CA125
USS (transvaginal / transabdominal)
Cytology of pleural fluid or ascitic fluidPathology (gold standard); this can be a CT-guided biopsy (e.g: from an omental deposit) OR a laparoscopy-guided biopsy of an abdominal ovary etc
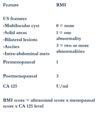
What is the RMI score?
Malignant Risk Index
RMI = ultrasound score x menopausal score x CA125 level
Patients with an RMI >200 should be referred to a gynae-oncology MDT
FIGO staging of ovarian cancer?
Stage I - confined to 1/both ovaries
Stage II - spread beyond the pelvic within the abdomen
Stage III - spread beyond the pelvis, within the abdomen
Stage IV - spread into other organs, e.g: liver, lungs
Prognosis of ovarian cancer?
Worsens with progression to later stages
Patterns of spread of ovarian cancer?
Transcoelomic spread / peritoneal seeding within the pelvis; results in spread to abdominal cavity
Haematogenous spread to liver, lungs and brain; this is rare and occurs late but is usually more common with BRCA mutation
Occurrence of brain metastases in ovarian cancer?
<2%; if it occurs, consider a BRCA mutation
Types of ovarian cancer?
Vast majority (>90%) are epithelial cell tumours of the ovary:
- Serous
- Mucinous
- Endometrioid
- Clear cell
- Undifferentiated
<10% are germ cell, granulosa cell tumours
Treatment of ovarian cancer?
Surgery:
- Total abdominal hysterectomy (TAH) and bilateral salpingo-oophorectomy (BSO)
- Omentectomy
- Optimal debulking
Surgery AND chemotherapy (can be given before, after or before and after surgery)
Surgical management of early ovarian cancer?
Early stage epithelial ovarian cancer - routine systematic lymphadenectomy is not recommended
Retroperitoneal lymph node sampling should be considered as part of surgical staging for apparent early stage disease
NOTE - in women with stage Ia, grade 1 or 2 disease, fertility conserving surgery is an option, as long as the contralateral ovary appears normal and there is not evidence of omental or peritoneal disease
Optimal surgery for advanced ovarian cancer?
If surgery is done, the aim is to achieve complete cytoreduction
Use of neoadjuvant chemotherapy may be considered as an alternative to primary debulking surgery
Management of relapsed disease?
Surgery cannot be done for relapses, as the patient is not curable
In specific patient, with relapse epithelial ovarian cancer that is platinum-sensitive, secondary cytoreductive surgery may be appropriate and may improve overall survival; the aim is complete resection of all macroscopic disease
Use of chemotherapy for ovarian cancer?
CARBOPLATIN / paclitaxel
Relapse rates are high
Palliative chemotherapy:
- Carboplatin
- Paclitaxel
- Etoposide
- Others
Use of chemotherapy for early ovarian cancer?
All women with high-grade, early stage ovarian cancer should be considered for adjuvant chemo
For early stage disease, maintenance cytotoxic chemotherapy should not be given
Use of chemotherapy for advanced disease?
1st line chemo treatment of epithelial ovarian cancer should inc. a platinum agent, either in combo or as a single agent
CARBOPLATIN is the platinum drug of choice in both single and combo (other agent is paclitaxel)
i.e: the current 1st line chemo is 3 weekly carboplatin / paclitaxel
What is intraperitoneal chemotherapy?
Chemo that includes an intraperitoneal element it used in specific cases
NOT DONE IN THE UK, due to assoc. morbidity


