Biochem part deux Flashcards
(40 cards)
What path takes you from Phenylalanine to Epinephrine?
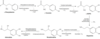
Phenlyalanine–> (Phenlyalanine hydrylase)–> Tryosine–> (tyrosine hydroxylase)–> DOPA–> (DOPA decarboxylase)–> Dopamine–> (Vit C)–> Norepinenphrine–> (SAM)–> Epinephrine
How do we get melanin production?
What wold cause albinism?
DOPA–> Melanin via Tyrosinase
INhibition of tyrosinase leads to albinism
Musty odor, ID, fair skin, exzema; obviously PKU. What’s the EnZ responsible?
What will increase in the body?
What AA becomes essential?
Due to Decreased phenylalanine hydroxylase or Decresaed tetrahydrobiopterin cofactor (malignant PKU). Tyrosine becomes essential. INCREASED phenylalanine –>excess phenylketones in urine.
Mom has low phenylaline hydroxylase and doesn’t monitor her diet during her pregnancy. What will happen to the baby as a result?
Mom has PKU:
Mom drinks lots of diet soda and shit with artificial sweatners
Findings in infant: microcephaly, intellectual disability, growth retardation, congenital heart defects
Mom is changing her babies diaper and notices it smells like burnt sugar. The doctor discusses nutritional changes to be made in the infants diet to deal with this including Isoluecine, Leucine and Valine. What’s the dx and enZ deficiency?
What are consequences if not given a strict diet?
What needs to be supplemented in the diet?
Maple Syrup Urine Diseaes: Blocked degradation of branched amino acids (Isoleucine, Leucine, Valine) due to DECREASED α-ketoacid dehydrogenase (B1).
Causes α-ketoacids in the blood, especially those of leucine.
Causes severe CNS defects, intellectual disability, and death.
Treatment: restriction of isoleucine, leucine, valine in diet, and thiamine supplementation.
You are doing in-patient rotations at the hospital and notice a nurse talking a urine sample from your pt who is there for horrible joint pain. The urine is BLACK and she’s explains she would expect it to be because it was sitting out for awhile, she was running behind.
What disease does this pt have?
What associated findings would possibly be present?
Congenital deficiency of homogentisate oxidase in the degradative pathway of tyrosine to fumarate–> pigment-forming homogentisic acid accumulates in tissue
Autosomal Recessive and often benign
dark connective tissue, brown pigmented sclerae, urine turns black on prolonged exposure to air. May have debilitating arthralgias (homogentisic acid toxic to cartilage).
You are rotating through optholmogy even though eyeballs are disgusting and a young tall man is brought in to clinic with his mother. He is very tall and intellectually disabled. He has been having vision issues and it is found he has a lens subluxation (downward and inward)
What pathway is disrupted in this patient?
What AA aren’t reabsorbed in this pt?
Homocystinuria :

HIGH homocysteine in urine, intellectual disability, osteoporosis, marfanoid habitus, kyphosis, lens subluxation (downward and inward), thrombosis, and atherosclerosis (stroke and MI)
Pt recently passes a kidney stone and the lab tells you its a cystein stone
What is the defect in your pts Kidney?
What AA are lost in the urine?
How do you tx your patient?

Hereditary defect of renal PCT and intestinal amino acid transporter that prevents reabsorption of Cysteine, Ornithine, Lysine, and Arginine (COLA).
Excess cystine in the urine can lead to recurrent precipitation of hexagonal cystine stones
Treatment: urinary alkalinization (e.g., potassium citrate, acetazolamide) and chelating agents (e.g., penicillamine) solubility of cystine stones; good hydration
Review the graph to get a feel for Glycogen regulation by insulin and glucagon
Glycogen: Branches have α-(1,6) bonds; linkages have α-(1,4) bonds.
see image

How is glycogen processed differently in the skeletal muscle vs hepatocytes
Muslces: Glycogen undergoes glycogenolysis–> glucose-1-phosphate—> glucose-6-phosphate, which is rapidly metabolized during exercise.
Hepatocytes:
Glycogen is stored and undergoes glycogenolysis to maintain blood sugar at appropriate levels. Glycogen phosphorylase liberates glucose-1-phosphate residues off branched glycogen until 4 glucose units remain on a branch. Then 4-α-d-glucanotransferase (debranching enzyme ) moves 3 molecules of glucose-1-phosphate from the branch to the linkage. Then α-1,6-glucosidase (debranching enzyme ) cleaves off the last residue, liberating glucose.
You pt had a recent episode of severe fasting hypoglycemia but has tested negative for diabetes. Labs show Increased Blood lactate, increased uric acid and high TGs. On physical exam you can palpate her liver.
Dx?
EnZ deficiency?
Tx?
Von Gierke Disease
Glucose-6-phostphatase deficiency
Little boy comes in with heart fail and ties. Labs show he died from an enZ deficiency. This disease is autosomal recessive.
Pompe disease: Lysosomal α-1,4-glucosidase (acid maltase) deficiency
Pompe trashes the Pump (and liver and muscle)
A mother brings her daughter into the office. The 10 yo recently joined a competitve soccer team and after the game had an episode of painless hematuria but her legs were very sore. What enZ deficiency could be responsible for pts condition?
McArdle Disease
Skeletal muscle glycogen phosphorylase (myophosphorylase) deficiency:
Increase glycogen in muscle, but muscle cannot break it down–> painful muscle cramps, myoglobinuria (red urine) with strenuous exercise, and arrhythmia from electrolyte abnormalities
Tx: B6 supplement
What mild form of glycogen disorder causes hypoglycemia,hyper TG but no change in blood lactate levels?
Cori Disease:
debranching enZ defient
Pt comes in with longstanding peripheral neuropathy (does not have diabetes) and recently has been having kidney issues. What EnZ deficiency could be causing his problems? What product would build up as a result?
Peripheral neuropathy of hands/feet, angiokeratomas, cardiovascular/renal disease.
Fabry Disease:
Deficient: α-galactosidase A
Build up: Ceramide trihexoside
(Ceira is a Fabulous Gal)
You are in the pathology lab and your attending points out a cell full of lipid laden macrophages that looks like wipspy paper. The note on the pt says that he has pancytopenia and is in the hospital for a femur fracture. What is the pts disease?
EnZ deficiency?
Build up?
Gauchers disease
Gaucher cells = crumpled tissue paper
Deficient: Glucocerebrosidase (β-glucosidase)
Build up: Glucocerebroside
Also see: Hepatosplenomegaly, pancytopenia,osteoporosis, aseptic necrosis of femur, bone crises, treatment is recombinant glucocerebrosidase.
60 yo pt comes in with his wife, he has progressive dementia and hepatosplenomegaly. During the PE you notice a red spot in the macula with the fundascope.
What’s the Dx?
EnZ deficiency?
Build up?
Niemman Pick
Sphingomyelinase deficiency
Spingomyelin buildup
(Progressive neurodegeneration, hepatosplenomegaly, foam cells (lipid-laden macrophages) “cherry-red” spot on macula )
*presents sim to Tay-Sachs; but Neimann Pick is longer name thus has larger organs!

Pt comes in with husband. She has cherry red spot on macula and has progressive dementia and normal AST/ALT. What do you Dx her with?
EnZ deficiency?
Buildup?
Tay-Sachs
Hexosaminidase-A
GM2 ganglioside
(simular to Niemann pick but NO hepatosplenomegaly)
4yo child comes in with mother… he points to his fingers and says they feel funny. The mother mentions concerns about that but also is concerned that he is smaller for his age and doesn’t seem to interact as well with other kids. You think it may be because he has really dorky glasses but don’t say anthing bc that would be rude.
Based on the pathology attached, what enZ is this pt most likely deficient in? What product build up is there?

Krabbe disease:
Deficient in Galactocerebrosidase
Build up of Galactocerebroside or psychosine
Peripheral neuropathy, developmental delay, optic atrophy, globoid cells
Young pt comes to the clinic with ataxic gait and dementia. The disesease she has causes central and peripheral demyleniation. What enZ deficiency is this and what build up product is there?
Metachromatic leukodystrophy
Arylsulfatase A defeiciency
Cerebroside sulfate build up
You are rounding in peds and a women brings her son in for a well-child. The baby is hideous, more then babies usually and has labored breathing. You can palpate the spleen and liver and notice corneal clouding. What is the EnZ defeiciency?
What is the buildup?
Hurler Syndrome: Mucopolysacchoridoses
Deficienct: α-L-iduronidase
Build up of: Heparan sulfate, dermatan sulfate
These children have developmental delay, gargoylism, airway obstruction, corneal clouding, hepatosplenomegaly.
You are at the grocery store and this little kid that looks like a gargoyle comes and kicks you in the leg for no reason then he punches his mom in the face. You think he for sure has an enZ deficiency, what is it?
What is the build up?
Hunter syndrome: (milder form of Hurler)
Deficient in: Iduronate sulfatase
Build up in: Heparan sulfate, dermatan sulfate
(Hunters see clearly (no corneal clouding) and aggressively aim for the X (X-linked recessive).
Long chain FA degradation requires ________ transport into the mitochondiral matrix.
IF this is deficiency we end up with toxic accumulation causing weakness, HYPOtonia, HYPOKETOTIC HYPOglycemia
Carnitine-dependent

What results when we have decreased Acyl-CoA dehydrogenase
Increased Dicarboxyclic acids, DECREASED glucose and ketones
Acetly-CoA is a +allosteric regulator of pyruvate caboyxylase in gluconeogenesis thus LOW actely-CoA = LOW fasting glucose


