FDN2_SM_WK4_EmbryologyPatternsDefects Flashcards
(134 cards)
What is the most common site of normal implantation?
Posterior wall of the uterus
What are some common sites of ectopic pregnancy?
Uterine tubule, cervix, abdominal cavity, ovary, etc
What are the major events of week 1 of embryogenesis?
Ovulation, conception, migration down the uterine tubule
Where does fertilization usually occur?
The distal 1/3 of the uterine tubule
What are the major events of week 2 of embryogenesis?
Implantation, extra-embryonic membrane formation
What stage is the conceptus when it implants?
Blastocyst
What are the components of a blastocyst?
Trophoblast = outer shell
Inner cell mass

What is the fate of the trophoblast?
It will:
- Differentiate into the outer syncytiotrophoblast and inner cytotrophoblast, then acquire its extraembryonic mesoderm layer (so the cytotrophoblast is now in the middle)
- When it has all 3 layers, it is called the chorion
- The villous chorion invade the endometrium and form the fetal components of the placenta
- The smooth chorion covers the amnion
How does the amnionic cavity form?
The blastocyst hollows to form two layers: The epiblast and the hypoblast

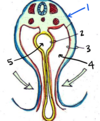
What is #1 pointing to?

Syncytiotrophoblast

What is #2 pointing to?

Amniotic Cavity

What is #3 pointing to?

Ectodermal amnion

What is #4 pointing to?

Epiblast/Ectoderm

What is #5 pointing to?

Hypoblast/Endoderm

What is #6 pointing to?

Trophobolast

The structure labeled by which number will eventually be in direct contact with maternal blood?

1 - the synytiotrophoblast
This layer will form the outermost part of the villious chorion that invades the endometrium and forms the fetal component of the placenta. It will be in direct contact with maternal blood from decidua basalis.

Name the 4 extra-embryonic membranes and their functions
Chorion: Villous forms the placenta, cmooth covers the amnion
Amnion: Surroudns embryo, will eventually fold down to form the cylinder
Yolk Sac: Provides early nutrition. Will become the first source of embryonic blood cells
Alantois: Vestigal membrane in humans
*Yolk Sac + Alantois become the umbilial cord
What is the final step in the formation of the 3 major extraembryonic membranes?
Extraembryonic mesoderm coats the old blastocyst cavity. Everything gets an “extra layer”
Trophoblast -> Chorion
Primary Yolk Sac -> Yolk Sac
Primary Amnion -> Amnion
Which embryonic structure forms the placenta?
The chorion (which came from the trophoblast)
Which embryonic structure forms the umbilical cord?
The yolk sac and the alantois
Which embryonic structure(s) form(s) the afterbirth?
The villous chorion (placenta) and the cytotrophoblastic shell
What is the major event of week 3 of embryogenesis?
Gastrulation (and subsequent formation of the intraembryonic mesoderm)
Describe the formation of the intraembryonic mesoderm
Induced by the primitive knot/node, which forms the primitive streak
Epiblast cells migrate through the invaginating primitive streak to first migrate into the hypoblast (displacing it), then create a layer of mesoderm in between the endoderm and ectoderm
From where does the intraembryonic mesoderm originate?
The primitive streak (epiblast cells migrate through it)