MOD F TECH 48 Maternity Flashcards
(67 cards)
Obstetric Emergencies
- Birth Imminent (Normal Delivery)
- Maternity Complications
It is essential that control are informed as soon as it is evident that an incident is maternity related and an ambulance crew are dispatched asap
The most important feature of managing an obstetric incident is a rapid and accurate assessment of the mother to ascertain whether there is anything abnormal taking place
Ambulance personnel will follow a maternal assessment process to decide on the dispositon of the mother i.e stay on scene and request a Midwife or transfer to further care immediately
Terminology
- EDD/EDB - estimated date of delivery / birth
- LMP - last menstrual period
- SB – still birth
- Primigravida / primip: 1st pregnancy
- Multigravida / multip: all subs. pregnancies
- G/Gravida: pregnant
- P/Para/parity: number of live births
- Gestation = length of pregnancy in weeks
- 0 – 40 weeks normal
- 37 – 42 term
- 24 – 37 pre-term
- 24 weeks and less – miscarriage
- Fundus: top of uterus
- Meconium – first stool baby passes, thick dark green and sticky
- VBAC – Vaginal birth after caesarean
Gestation
A pregnancy is divided into three ‘trimesters’ each of 13 weeks. It is important to establish the stage in the pregnancy (Measured in weeks of duration of the pregnancy) to inform the crew to determine their course of action. For example, 14/40 on a maternity plan means that the mother is 14 weeks into the 40 week duration of pregnancy
General and Local Organisation of Obstetrics and Gynaecology Services

Stages of Labour
- First stage - the longest part of labour. The cervix is dilating (Opening up) during this stage
- Second stage – starts when the cervix is fully dilated (10cm) and ends with the delivery of the baby
- Third stage – Expulsion (Delivery) of the placenta and membranes
3 stages of Labour

Indicators of the onset of Labour
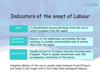
Imminent Delivery Indicators
•Regular contractions at 1-2minute intervals and an urge to push or bear down
•
•Crowning or the top of the babies head/breech presentation visible at the vulva
Indicators of second stage

Management of second stage of labour
- Ask Control to arrange for a midwife or second vehicle/Paramedic to attend if you haven’t yet moved from the home address
- Prepare trolley bed or delivery area with incontinence pads
- Reassure the mother and tell her what you are doing. Remember to include the woman’s partner if present
- Have towels ready, enough to dry the baby and another to wrap the baby
- Support the mother in a semi-recumbent (or other comfortable) position discouraging her to lie flat on her back to avoid supine hypotension
- Encourage her to continue taking entonox to relieve pain and discomfort
- Open and lay out maternity pack
- Cover mother with blanket for warmth and modesty
- Respect ethnicity, religious and personal beliefs in respect of modesty i.e. some women will find it distressing to be attended by males
- As the baby’s head is delivering get the mother to pant rather than push. Instruct the mother to pant or puff allowing the head to advance slowly with the contraction. Consider applying gentle pressure to the top of the baby’s head as it advances through the vagina to prevent very rapid delivery of the head
- Check to see that the umbilical cord is not wrapped around the baby’s head; if it is, you may gently attempt to loop it over the head. If it is too tight leave it where it is; a tight cord should not prevent the baby delivering
•
•Quickly dry the baby when it is completely delivered wiping any obvious large collections of mucous from the baby’s mouth and nose
•
•Wrap in a dry towel and place the baby on the mothers abdomen
Only cut the cord if the following applies
•Mother or newborn requires resuscitation or medical intervention; examples of risk factors include: pre-term babies or haemorrhage
•
•Short umbilical cord where the baby cannot be placed on the mothers abdomen
•
(EMAS Clinical Bulletin 05/12/10 issue 15 – supersedes JRCALC guidance)
Third stage of labour

Third stage of labour
Deliver the placenta into a bowl or plastic bag and retain all discharge for inspection by a Doctor or Midwife

Management of the third stage of labour
- Do not pull on the cord during delivery of the placenta as this could rupture the cord making delivery difficult and cause excessive bleeding or inversion of the uterus
- If bleeding continues after delivery of the placenta massage the top or fundus of the uterus (at the level of the umbilicus) with a cupped hand, using a circular motion. This should become firm as gentle massage is applied. Consider the use of entonox to relieve associated pain and discomfort
Newborn assessment
•Place the baby on mother’s abdomen, dry and cover. The mother can assist by holding the baby securely
•
•Assess the newborn based on three factors
–Colour
–Heart Rate
–Respiration
Newborn assessment

Immediate Care
Warmth
Babies are extremely vulnerable to heat loss
Assess APGAR
Primary cause of a floppy baby at birth is hypoxia
Warmth
Babies are extremely vulnerable to heat loss
Assess APGAR
Primary cause of a floppy baby at birth is hypoxia

Pink, Blue, White baby
A healthy baby (Pink) will:
- be born BLUE but will ‘pink up’ rapidly
- have good tone
- cry within a few seconds
- have a good heart rate (120-150) within a few minutes.
Pink, Blue, White Baby
A less healthy baby (blue) – primary apnoea
- Born blue
- less tone
- May have a slow heart rate (<100)
- May not establish adequate breathing by 90-120 seconds after birth.
Pink, Blue, White Baby
An Ill baby (white) – terminal apnoea
- Born pale and floppy
- Not breathing
- Slow, very slow or undetectable heart rate (<60)
Airway
Before a baby can breathe effectively the airway must be open.
–Is baby’s head in neutral?
–Do you need a jaw thrust?
–Do you need a second person’s help to maintain neutral?
These manoeuvres will be effective for the majority of babies requiring airway stabilisation at birth.
Suction?
Airway suction immediately following birth should be reserved for babies who have obvious airway obstruction that cannot be rectified by appropriate positioning.















