Red Blood Cells Flashcards
(58 cards)
Where do all blood cells originate from
Bone marrow
Where are the blood cells derived from
Haemopoietic stem cells
What gives rise to erythrocytes
Myeloid stem cells
Table of the blood cells

What are the HSC characteristics
Self-renew (daughter cells remain as HSC)
Differentiate to daughter cells
Stem cell hierarchy

Where are HSC developed in fetus
3 wks in the mesoderm (yolk salk)
6-8 wks liver takes over and remains principal until shortly before birth
10 wks bone marrow
Where is HSC developed in children
Bone marrow everywhere
Where is HSC developed in adults
Pelvis, femur, sterum and proximal arm and thigh
Other sites may retain their ability
Haemopoiesis may occur outside the bone marrow
What is haemopoiesis regulated by
Genes, transcription factors, growth factors and microenvironment
What are haemopoietic growth factors
Glycoprotein hormones which bind to cell surface receptors
Regulates proliferation and differentiation of HSC
Regulate function of mature blood cells
What is the role of erythropoietin
Induces erythropoiesis
Synthesised in the kidney
Glycoprotein
Stimulates bone marrow to produce more red blood cells
Direct cause or reduced oxygen to the kidney
How are granulocytes and monocytes regulated
G-CSF
Granulacyte Macrophage Colony Stimulating Factors
Cytokines e.g. interleukins
What is the role of thromopoietin
Platelet production
Megakaryocytopiesis
Produced by cells of the bone marrow
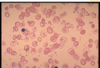
Development of red blood cells

Why do we need iron
Oxygen transport in haemoglobin
DNA synthesis
Mitchondrial proteins
Where is haem iron (Fe2) found
Red meat
Fish
Where is non-haem iron found
Grains
Beans
Plant based food
Dairy
Nuts
Soya beans - contains phytates which reduce iron absorption
What reducing substances are required to absorb non-haem iron
Ascorbic acid
Vitamin C
Why is it important to regulate iron absorption
Iron can form free radicals which can damage tissues
What is the molecule that transports iron
Transferrin
What is hepcidin
Regulates absorption of iron
Ferroportin - Fe3
Ferritin - Fe2
Iron is shed into the gut lumen otherwise

What cytokines are produced in inflammatory response
IFNy - reduction in erythropoiesis
IL-1 TNFa and IL-6 mediate hepcidin
How does hepcidin cause anaemia?
Prevent uptake of iron