Immunodeficiency Diseases Flashcards
What do we mean by immunodeficiency?
- Infections that are…….
- O..
- U..
- Unusually …, … or not responding to … …
- F…
- Infections that are…….
- Opportunistic
- Unusual
- Unusually severe, protracted or not responding to standard therapy
- Frequent
Immunodeficiency - difficulty in defining

- So there is no definitive definition…….
- The diagnosis is largely descriptive
- Infections more likely to be significant if……..
- Infections are verified rather than simply reported
- Organisms can be identified
- End-organ damage has occurred
Infections more likely to be significant if…. (3)
- Infections are verified rather than simply reported
- Organisms can be identified
- End-organ damage has occurred
General classification of immunodeficiency
- … immunodeficiency
- … immunodeficiency …
-
Secondary immunodeficiency
- Immune defect is secondary to another disease process
- Very common
- Extremes of age
- Malignancies (esp myeloma, lymphoma)
- Metabolic eg diabetes
- Drugs eg chemotherapy, steroids
- Infection eg HIV
-
Primary immunodeficiency syndrome (PID)
- Immune defect is intrinsic to the immune system itself
- Rare
- Often genetic, but not always
- Over 100 characterised PIDS
- Mostly are fairly ‘new’ diseases
- Fatal in pre-antibiotic era
- Characterisation required developments in technology
Secondary immunodeficiency
- Immune defect is secondary to another disease process
- Very …
- Extremes of …
- … (esp myeloma, lymphoma)
- … eg diabetes
- … eg chemotherapy, steroids
- … eg HIV
- Immune defect is secondary to another disease process
- Very common
- Extremes of age
- Malignancies (esp myeloma, lymphoma)
- Metabolic eg diabetes
- Drugs eg chemotherapy, steroids
- Infection eg HIV
Primary immunodeficiency syndrome (PID)
- Immune defect is … to the immune system itself
- …
- Often …, but not always
- Over … characterised PIDS
- Mostly are fairly ‘…’ diseases
- … in pre-antibiotic era
- Characterisation required developments in …
- Immune defect is intrinsic to the immune system itself
- Rare
- Often genetic, but not always
- Over 100 characterised PIDS
- Mostly are fairly ‘new’ diseases
- Fatal in pre-antibiotic era
- Characterisation required developments in technology
Immunological classification of immunodeficiency


Immunological classification of immunodeficiency


More notes on immunodeficiency……..
- CD… T cell defects affect B cells, as T cell help is need for B cell maturation
- This is particularly marked in …; less marked in …,
- Immunodeficiency syndromes affecting both antibody production and T cells are called … …
- In addition to infections, many immunodeficiency syndromes manifest with immune …: uncontrolled …, … diseases
- CD4 T cell defects affect B cells, as T cell help is need for B cell maturation
- This is particularly marked in infants; less marked in adults, who have already matured their B cells
- Immunodeficiency syndromes affecting both antibody production and T cells are called combined immunodeficiencies
- In addition to infections, many immunodeficiency syndromes manifest with immune dysregulation: uncontrolled inflammation, autoimmune diseases
More notes on immunodeficiency……..
- CD4 T cell defects affect B cells, as T cell help is need for B cell …
- This is particularly marked in infants; less marked in adults, who have already … their B cells
- Immunodeficiency syndromes affecting both … production and T cells are called combined immunodeficiencies
- In addition to infections, many immunodeficiency syndromes manifest with immune dysregulation: … inflammation, autoimmune diseases
- CD4 T cell defects affect B cells, as T cell help is need for B cell maturation
- This is particularly marked in infants; less marked in adults, who have already matured their B cells
- Immunodeficiency syndromes affecting both antibody production and T cells are called combined immunodeficiencies
- In addition to infections, many immunodeficiency syndromes manifest with immune dysregulation: uncontrolled inflammation, autoimmune diseases
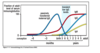
Aging and immunity (‘immunosenscence’)
‘A combination of age-related changes in the immune system that result in greater … to infection and reduced response to …’
‘A combination of age-related changes in the immune system that result in greater susceptibility to infection and reduced response to vaccination’
What is ‘immunosenscence’?
‘A combination of age-related changes in the immune system that result in greater susceptibility to infection and reduced response to vaccination’
Some immunological aspects of immunosenescence
- Thymic …
- Telomere … in stem cells reduces both quality and quantity of leucocyte output
- Reduced T and B cell receptor …
- Reduced … responses
- Reduced neutrophil function
- Reduced self-tolerance; inflammation switches from protection to damage
- Expansion of T cell pool responding to cytomegalovirus (current research focus)
- Thymic involution
- Telomere shortening in stem cells reduces both quality and quantity of leucocyte output
- Reduced T and B cell receptor diversity
- Reduced vaccine responses
- Reduced neutrophil function
- Reduced self-tolerance; inflammation switches from protection to damage
- Expansion of T cell pool responding to cytomegalovirus (current research focus)
Some immunological aspects of immunosenescence
- Thymic involution
- Telomere shortening in stem cells reduces both quality and quantity of leucocyte output
- Reduced T and B cell receptor diversity
- Reduced vaccine responses
- Reduced … function
- Reduced …-…; inflammation switches from protection to damage
- Expansion of T cell pool responding to … (current research focus)
- Thymic involution
- Telomere shortening in stem cells reduces both quality and quantity of leucocyte output
- Reduced T and B cell receptor diversity
- Reduced vaccine responses
- Reduced neutrophil function
- Reduced self-tolerance; inflammation switches from protection to damage
- Expansion of T cell pool responding to cytomegalovirus (current research focus)
Elderly clearly more susceptible to infection, but immunity itself is not the only factor:
- Reduced …
- n…
- … healing
- Co-… (COPD, CCF, DM, cancer, depression etc)
- Reduced … reserve
- All of these increase … of infection AND risk of poor … from infection
- See VZV immunisation slides: clear that older people can make a response to a specifically tailored immune booster
- Reduced mobility
- Nutrition
- Wound healing
- Co-morbidities (COPD, CCF, DM, cancer, depression etc)
- Reduced physiological reserve
- All of these increase risk of infection AND risk of poor outcome from infection
- See VZV immunisation slides: clear that older people can make a response to a specifically tailored immune booster
Predominantly antibody deficiency
- Low Ig…; other isotypes may be affected, but low IgA/ M with normal … is rarely significant
- Manifests with recurrent … infections of the upper and lower respiratory tract
- Sometimes … infections in addition
- Infections typically respond to anti-…, but response may be sub-optimal and long courses required
- If untreated, leads to irreversible lung damage (…)
- Low IgG; other isotypes may be affected, but low IgA/ M with normal IgG is rarely significant
- Manifests with recurrent pyogenic infections of the upper and lower respiratory tract
- Sometimes gut infections in addition
- Infections typically respond to anti-microbials, but response may be sub-optimal and long courses required
- If untreated, leads to irreversible lung damage (bronchiectasis)
Predominantly antibody deficiency
- Low IgG; other isotypes may be affected, but low IgA/ M with normal IgG is rarely significant
- Manifests with … pyogenic infections of the …and … … tract
- Sometimes gut infections in addition
- Infections typically respond to anti-microbials, but response may be …-optimal and … courses required
- If untreated, leads to … lung damage (bronchiectasis)
- Low IgG; other isotypes may be affected, but low IgA/ M with normal IgG is rarely significant
- Manifests with recurrent pyogenic infections of the upper and lower respiratory tract
- Sometimes gut infections in addition
- Infections typically respond to anti-microbials, but response may be sub-optimal and long courses required
- If untreated, leads to irreversible lung damage (bronchiectasis)