Chapter 52: Portal Hypertension Flashcards
Where does the portal vein begin?
At the confluence of the splenic vein and the SMV
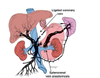
What are the six potential routes of portal–systemic collateral blood flow (as seen with portal hypertension)?
- Umbilical vein
- Coronary vein to esophageal venous plexuses
- Retroperitoneal veins (veins of Retzius)
- Diaphragm veins (veins of Sappey)
- Superior hemorrhoidal vein to middle and inferior hemorrhoidal veins and then to the iliac vein
- Splenic veins to the short gastric veins
What is the pathophysiology of portal hypertension?
Elevated portal pressure resulting from resistance to portal flow
What is the etiology?
Prehepatic
Thrombosis of portal vein/atresia of portal vein
What is the etiology?
Hepatic
- Cirrhosis (distortion of normal parenchyma by regenerating hepatic nodules)
- hepatocellular carcinoma
- fibrosis
What is the etiology?
Post hepatic
Budd–Chiari syndrome: thrombosis of hepatic veins
What is the most common cause of portal hypertension in the United States?
Cirrhosis (>90% of cases)
How many patients with alcoholism develop cirrhosis?
Surprisingly, <1 in 5
What percentage of patients with cirrhosis develop esophageal varices?
≈40%
How many patients with cirrhosis develop portal hypertension?
≈2/3
What is the most common physical finding in patients with portal hypertension?
Splenomegaly (spleen enlargement)
What are the four associated CLINICAL findings in portal hypertension?
- Esophageal varices
- Splenomegaly
- Caput medusae (engorgement of periumbilical veins)
- Hemorrhoids

What other physical findings are associated with cirrhosis and portal hypertension?
- Spider angioma
- palmar erythema
- ascites
- truncal obesity and peripheral wasting
- encephalopathy
- asterixis (liver flap)
- gynecomastia
- jaundice
What is the name of the periumbilical bruit heard with caput medusae?
Cruveilhier–Baumgarten bruit
What constitutes the portal–systemic collateral circulation in portal hypertension in the following conditions:
Esophageal varices?
Coronary vein backing up into the azygous system
What constitutes the portal–systemic collateral circulation in portal hypertension in the following conditions:
Caput medusae?
Umbilical vein (via falciform ligament) draining into the epigastric veins