Case 01 Flashcards
(14 cards)

Patient is a 39-year-old recreationally active female who had a positive response to her right knee MACI/AMZ for patellofemoral chondral disease and desired to pursue the same treatment for her symptomatic left knee 6 months prior
Patient has a significant past medical history for chronic pain, work-related low back injury, previous gastric bypass, former college athlete.

Patient complained of bilateral anterior knee pain with significant exacerbating patient going up and down stairs, difficulty with recreational activities and moderate to severe pain.
She had undergone greater than 9 months of conservative treatments to include anti-inflammatories as tolerated as she had gastric bypass, intra-articular cortisone injections and physical therapy.

Patient is 6ft 1, 250lbs for a BMI of 32
Left knee examination upon initial inspection is concerning for patellofemoral pathology. There is no obvious deformity noted. No previous scars. There is tenderness upon palpation throughout the patellar tendon region in the patella itself, and the medial and lateral joint lines. I appreciate a subtle effusion. Some crepitus identified. Passive Range of Motion is 0-140 degrees and active is 0-140 degrees. Strength assessment is 5/5 in the quadriceps, 5/5 in the hamstrings. Mild to moderate VMO deficiency. Negative anterior and posterior drawer exam. Negative Lachman exam. Stable to Varus and Valgus stress testing. Negative McMurray´s exam. Negative Apley compression test. Negative J-sign, A cursory skin inspection is normal with palpable distal pulses.
Xrays were normal/preoperative lab work was normal as well
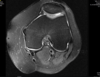
Superficial fissuring of the lateral patellar facet cartilage, normal patellar ratios, TTTG 26mm
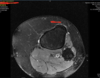

Isolated 2cm2 grade 4 chondral defect of the lateral patella facet with a normal trochlea.
Patient already had success with her right knee procedure we wanted to perform a similar procedure. She was aware of the significant pain and downtime of the cartilage transplant as well as anticoagulation
she felt that she had recovered enough strength and function to be able to compensate on her recently operated right side.
The patient had a normal medial facet and elevated TT TG which would fit criteria for anterior medialization which in conjunction with a MACI procedure would likely provide the most, biomechanical optimization for the health of her knee and cartilage long-term.
In addition she wanted to perform a MACI procedure as this autograft cellular based, and tissue engineering on a collagen scaffold.

Surgical technique was a combined cartilage transplant and anterior medialization. Made a large incision the superior patella down distal to the tibial tubercle:. I created soft tissue flaps down to the knee and proximal tibia. As this was an anterior medialization I set my osteotomy at 45 degrees to both medially and anteriorly transfer the tibial tubercle. I made my cuts in the tibia and as this was a in conjunction with a patella cartilage transplant I excised the tibial tubercle and made a medial arthrotomy to fully expose the patella.
I then used the cartilage cutting blocks to size the appropriate cartilage block transfer. I used a scalpel and curette to excise damaged cartilage debrided to stable healthy rims. I then cut a similar size patch on the MACI graft on the back table. I then used fibrin glue to sandwich the graft into the patella defect and allowed the requisite time to allow the fibrin glue to stabilize the graft.
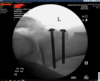
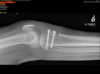
Next. I used intra-operative fluoroscopy to localize my tibial tubercle transfer. My goal was to elevate -1-2cm and medialize 1-2 cm. I measured this intra-operatively then placed two Steinman pins proximally and distally in the tibial tubercle graft through the posterior cortex. I was then able to use fluro and Measure the screw distances. The screws, in sizes of 5 so I found the appropriate screws, added a washer. The screws are self-tapping so use power then and to ensure excellent compression at the ostomy site. I then used fluoroscopy to confirm appropriate hardware localization. Tourniquet time was 65 minutes with an estimated blood loss of 20 mL.
Patient was discharged to home from the PACU. In the middle of the night she paged me as part of the on-call service with concerns of uncontrolled bleeding. Told her to go to the emergency room for further evaluation. The emergency room physician took down the sterile dressing and found there is no acute blood bleeding.
I then saw her in the office that day why I evaluated the wound and found again no active bleeding but serous oozing over superficial area that I placed a reinforcement stitch to stop the bleeding bleeding and oozing. Then sent the patient to the lab to measure her hematocrit. It was 30.

Patient was seen 14 days later in the office foutine postoperative visit. They are functionally doing well without fevers chills night sweats and good pain control. There was no drainage or signs of infection.
6 days later the patient came to the office for an unscheduled visit. She had what appeared to be a superficial wound dehiscence with drainage at the inferior border. This was in the setting of the Covid crisis with an anticipated foreclosure and shelter in place pending. The patient was admitted through the emergency room and taken to the operating room that day.
The patient was taken to the OR and placed in the supine position. Antibiotics were withheld. Using the inferior aspect of the incision I created soft tissue flaps. I dissected down deep and identified a large amount of hematoma at the osteotomy site. The hematoma extended all the way up superficial to the knee joint but did not involve intra-articular compartment.
I took cultures both at the superficial and deep and I irrigated the wound with normal saline and gave antibiotics.
Traditionally we will keep patients in the hospital to monitor cultures and IV antibiotics. This is atypical in the impending Covid crisis. Thus patient was discharged on oral clindamycin with close follow-up and a discussion with the ID doctors. Importantly the orthopedic surgeons record quarantine off care so this was primarily managed by the PAs.
Both superficial and deep cultures grew out MSSA.
Patient had continued wound drainage and an incisional wound VAC was placed. By this time there was a statewide plan on elective surgeries.

For two weeks the patient had progressive drainage on antibiotics. She was also anemic (hct 28)CRP .8/ESR 59, and anxious with the covid crisis. The wound was dehiscing and malodorous.
We had a team meeting to return to the OR, bone biopsy/culture, screw exchange if possible and admission for picc line insertion and IV antibiotics. Patient was deeply concerned about having the screws and and also being hospitalized in the Covid crisis and catching Covid.
Moreover we were in a crisis worker surgeries were not allowed and will oftentimes did not have the appropriate supplies both PPP and general surgical supplies to perform this.

Identified gross pus deep, and the screws were loose. The osteotomy was now at 5 weeks so it was relatively solid but I did not want to go without fixation so I exchanged the screws.
Deep drain and incisional wound vac was placed. Patient was admitted, PICC line placed, ID prescribed IV Vancomycin with telemedicine follow-up. MSSA, finegoldia magna, added flagyl
Return to OR for wound closure
Unfortunately, the drainage was so much that the incisional wound vac would fill and the patient could not manage it. We were able to arrange for VNA to cover incisional wound vac changes during this time so we returned to the OR for a repeat I and D and incisional wound vac placement. Also in the setting of an escalating crisis and surgery ban. Surgeries required chairman approval . I again took her to the operating room where I performed excisional debridement, found generally healthy tissue without evidence of pus the tibial site was intact and soft tissues were able to cover the hardware. I then placed a deep wound VAC deep over at the surgical site at the tibia.
Patient was able to tolerate the wound VAC for 6 weeks with changes at the VNA and in consultation with wound care. After 6 weeks she was intolerant of the wound VAC and wanted to proceed with a primary closure with possible allograft augmentation for any areas of granulation in conjunction with wound care clinic guidance. This time the granulation looks healthy and viable. Hardware was covered. And I was able to close primarily without tension no need for allograft. The patient was discharged to home off antibiotics and generally feeling well.
Postoperatively the patient was concerned about another hematoma so I ordered an ultrasound which confirmed a recurrent hematoma. When the procedure with radiology under sterile technique there was no not able to aspirate any fluid using ultrasound guidance.

Patient was also concerned about the remaining screws so we ordered a CT scan to assess healing. Interval callus formation so we added a bone scan


1 year later the patient was doing well with her knee surgery. Wound has closed, her pain is resolved and she is functioning doing well.
She had to undergo emergent neck and back surgery in the recovery period which was delaying her overall progression and had some generalized fatigability but she is generally happy with the knee at 1 year out



