Case 09 Flashcards
(11 cards)
HPI

Patient is a 56yo RHD housekeeper/weightlifter who presented with failed massive arthroscopic rotator cuff repair for 1 year with persistent pain and functional deficitswho elected to undergo revision arthroscopic rotator cuff repair after failure of conservativetreatments and a second opinion.
Relevant past medical history: 1/10/19 s/p Left shoulder arthroscopic rotator cuff tear (supra, infra,subscap tear repair withTOE repair technique, subacromial decompression with subpectoral biceps tenodesis.
Bodybuilder/Housecleaner/Medically healthy non-smoker
PE
At 6M s/p primary repair—Left shoulder examination, upon initial inspection, is concerning for rotator cuff pathology.
With active arm elevation, I witness moderate scapulothoracic dyskenesis. There is tenderness to palpation throughout the insertion point of the supraspinatus tendon at the proximal humerus, as well as at the bicipital groove, but not with compression of the AC joint.
Passive range of motion is full, with forward flexion at 180 degrees, abduction 170 degrees, ADDER less than 90, ABDER 70 degrees, and Internal rotation to L3. Active range of motion is Limited, with forward flexion and abduction limited., ADDER less than degrees, ABDER 70 degrees, and Internal rotation to L3.
Strength assessment is 4+/5 in the supraspinatus, 5/5 Infraspinatus, 5/5.
Second Opinion
SCR
Tendon transfer
Reverse
Partial repair
Continued therapy
s/p TOE
concern over tear at musculotendon junction
no atrophy
weightlifter/young

We ordered an MR arthrogram to characterize her healing demonstrated a complete retear after a massive rotator cuff repair and biceps tenodesis at the supraspinatus with likely failure at the musculotendinous junction after transosseous equivalent repair.
I was also concerned that it appeared that she had retraction to the glenoid, joint incongruity, but was also without significant atrophy in the supra and infra spinatus.
recognized as a challenging surgical problem and got help.
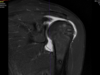

MRarthrogram
Loss of supra insertion
no significant atrophy

surgical decision making
- Failed non-op 6M
- Tear at Junction/massive
- Weightlifter
- No atrophy
- not keen on allograft
tendon transfer?

- Surgical decision-making was complex. Patient is a 57-year-old female with significant activity requirements is a body builder but also functional demands as a housekeeper. She is only 6 months status post massive rotator cuff repair with a transosseous equivalent repair technique and I was concerned that she had a rupture at the musculotendinous junction.
- Moreover she had a shoulder at risk with joint incongruity but she did demonstrate no significant atrophy of the muscles.
- She is not amenable to an arthroplasty as she wanted to continue working out as this was an important part of her identity.
- Moreover she was amenable to continued therapy and observation for 6 months after the MRI is a nonsurgical alternative especially as she will be traveling out of the country.
- The patient eventually decided to pursue with revision rotator cuff repair. She did not want to proceed with muscle transplant, SCR or arthroplasty.
She was amenable to both of us participating in the surgery, given the complexity and the desire to optimize her situation.

Surgical technique (5 points)
- balance cuff with subscap repair
- medialize footprint
- release adhesions
- L shaped tear
- Conservative recovery protocol
subscap repair
mason allen fiber tape stitch with lysis of adhesions
biceps groove as anatomic landmark
mason allen fiber tape stitch with lysis of adhesions
biceps groove as anatomic landmark
I Felt the supscap was repairable with adhesion release and a single anterior suture leading edge repair with a mason allen stitch configuration with the anchor placed near the biceps grove for anatomic length tensioning.

- Anterior leading edge L shaped tear
- Medialized the footprint
- release adhesions to mobilize tendon remnant
- two medial row anchors mason allen suture repair


I identified the supraspinatus as a L-Shaped tear with integrity of the the infraspinatus.
I performed a subacromial decompression to release the adhesions off of the acromion.
I medialized the footprint and placed 2 single row anchors with mason allen stitch configurations to reapproximate the tendon tear.


Follow-up
2/6W
6M/1YR

Surgical time with 135 minutes with minimal blood loss.
The patient was given a sling/multimodal pain medications and a conservative rehab protocol.
Patient general postop course was uncomplicated. I saw her at 2 weeks and6 weeks; Covid restrictions interfered with routine follow-up.
She was then seen in the office at 6M and functionally doing well. Patient was seen at 1 year follow-up and was also doing great. Wanted ultrasound or MRI for reassurance.


