Case 08 Flashcards
(9 cards)

82 yo male presents with 3 months history of severe left knee pain after a
traumatic fall on his left side in his backyard in August. Initial positive response to intraarticular cortisoneinjections then HEP but with persistent mechanical symptoms and failure of conservative treatmentoptions. NSAIDS contraindicated.
Patient had a fall in his backyard in August while carrying branches and is initially treated and released in the emergency room. He followed up with his primary care doctor who treated him conservatively with activity modification and rest. He had a working diagnosis of an MCL sprain.
Patient presented to me approximately 2 months after traumatic etiology with persistent severe knee pain with mechanical type symptoms. We treated him with intra-articular cortisone injection. Patient return to the office in 2 weeks with good results. And again at 6 weeks follow-up

Left knee examination upon initial inspection is concerning for meniscal pathology. There is no obvious deformity noted. No previous scars. There is no tenderness upon palpation throughout the patellar tendon region and in the patella, but with primarily medial and lateral joint line tenderness. I appreciate a subtle effusion. Passive Range of Motion is 0-140 degrees and active is 0-140 degrees. Strength assessment is 5/5 in the quadriceps, 5/5 in the hamstrings. Negative anterior and posterior drawer exam. Negative Lachman exam. Stable to Varus and Valgus stress testing. Positive McMurray´s exam. Pain is recreated with deep knee flexion Positive Apley compression test.

Relevant past medical history: Atrial fibrillation (Acute) CHF (congestive heart failure) (Acute)
Diabetes (Acute) Diabetic neuropathy (Acute) GERD (gastroesophageal reflux disease)
Gout (Acute) Hyperlipidemia (Acute) Hypertension (Acute) Kidney disease (Acute) On elliqus for Anticoagulation
I ordered it in office Rosenberg view to fully characterize whether this was occult medial compartment arthrosis vs meniscal or loose body pathology.
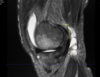
3 months after his initial injury an MRI was ordered to further characterize his knee pain. The MRI was most notable for subchondral edema in the medial femoral condyle, medial meniscal tear, medial femoral condyle chondrosis and 2 loose bodies in the intercondylar notch anterior knee with a significant effusion.

He had significant pain, mechanical symptoms, swelling for 3 months or more after traumatic etiology and failure to return back to his normal activities. In addition we anticipated addressing any potential unstable chondral flaps or meniscal tears.
We also reviewed conservative treatment options and we felt that we had exhausted those approaches. He was discharged from physical therapy, he could not take any anti-inflammatories, cortisone injection with incomplete, he had moderate to severe pain and mechanical symptoms with swelling.
He sought medical clearance and elected to proceed with arthroscopy.

Performed comprehensive diagnostic arthroscopy. I evaluated the gutters for loose body I did not document visualization of the posterior compartment nor the medial meniscus tear. I did characterize the medial meniscal tear of absent any unstable flaps and did not warrant meniscal debridement. I did identify significant stenotic synovitis throughout the joint which underwent a synovectomy I also found a small areas of loose body that was less than 5 mm which I felt was broken up loose bodies. Had significant gapping in the lateral compartment which of poor performance of serial debridements to see if I can retrieve any loose bodies posteriorly however I did not place a trocar into the notch posteriorly to exclude any loose bodies there.

Performed arthroscopic synovectomy using a rotary shaver. In the suprapatellar pouch did not find numerous small loose bodies did not feel criteria to code as a loose body.
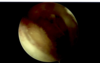

The medial compartment I did not identify an abnormal meniscus, I did see unstable cartilage flaps in the medial femoral condyle that elected to perform a chondroplasty using a rotary shaver.
I then completed the diagnostic arthroscopy without any additional pathology identified. Duration of surgery was 35 minutes with 15cc estimated blood loss.
Patient was discharged with multimodal pain meds, limited narcotics, aspirin and ice/crutches, WBAT, routine knee arthroscopy protocol.

Post-op Follow-up
2+6= *8
Patient general postop course was complicated by the covid shutdown. I saw him at 2 weeks, 6 weeks in the office where his recovery was routine. at the anticipated postoperative period I reached out to him to see how is doing.
He is not amenable to coming into the office or did not feel the need to do a telemedicine visit as he is generally doing well and happy with his recovery.


