Case03 Flashcards
(11 cards)

Patient is a 36-year-old recreationally active man who is sustained an acute left knee injury while playing softball. He felt a pop and significant swelling and inability to play. He has significant past medical history of an ACL reconstruction performed approximately 18 years ago.
Patient was recreationally active, medically healthy and works as a truck driver

left knee examination upon initial inspection is concerning for knee instability. There is no obvious deformity noted. There is tenderness upon palpation throughout the patellar tendon region and in the patella, but with primarily medial and lateral joint line tenderness. I appreciate a subtle effusion. Passive Range of Motion is 0-140 degrees and active is 0-140 degrees. Strength assessment is 5/5 in the quadriceps, 5/5 in the hamstrings. Positive Anterior drawer exam. IIB Lachman exam. Apprehension with pivot exam. Stable to Varus and Valgus stress testing. Equivocal McMurray´s exam. Negative Apley compression test. Negative J-sign, A cursory skin inspection is normal with palpable distal pulses.
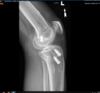
X-rays were reviewed and is most notable for previous ACL reconstruction with appropriate tibial tunnel and a previous metal interference screw, and it to my interpretation is a vertical femoral tunnel with cortical fixation device, no significant radiographic evidence of tunnel osteolysis or hardware failure.
Clinically I was concerned about the integrity of the ACL so we ordered an MRI the radiologist interpreted normal and intact

Radiology report noted an intact ACL and lateral meniscal tear with extrusion.
My interpretation of the ACL I was concerned about his loss of overall integrity especially given the bone bruising in the proximal tibia.

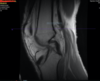
I also was able to better interpret the tunnel placement as well as absence of any tunnel osteolysis.


Patient return to me in the office will with still persistent instability despite physical therapy.
Based on the patient’s repeated complaints of stability in the setting of a questionable ACL and meniscal tear, resumption of his quadricep range of motion at the initial injury I indicated the patient for left knee examination under anesthesia right stress test the ACL, diagnostic arthroscopy, anticipated meniscectomy versus repair and anticipated anterior cruciate revision reconstruction with bone tendon bone allograft.
Specifically I felt the tibial tunnel is one that I could reduce there is no significant osteolysis has appropriately placed. I was also anticipating an anatomic or anterior medial portal would be sufficient and not intervene with the vertical femoral tunnel placed previously. I would also be prepared with both cortical fixation devices as well as interference after fixation technique as well. In regards to the lateral meniscus I was prepared for both debridement, arthroscopic repair stitches with the outside possibility of an open repair however given the extrusion this was likely very low probability.
We spoke about graft choices with the patient; patient was a truck driver and wanted to get back to driving quickly did not want to have an extended recovery. He has no concerns about using allograft tissue so we decided to use bone tendon bone allograft which is my mainstay graft choice something I feel comfortable with technically.
Nonoperative: Physical therapy, quad strengthening, ACL brace, cortisone injections, activity modification
single stage vs staged approach, chondroplasty vs joint preservation procedures, osteotomies


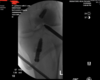
Surgical complication representing was a failure of hardware with resultant metal loose body in the joint identified. At the time of femoral reaming with a new a 10 mm low-profile reamer a piece of metal drill broke off. This was identified at the completion of reaming when we inspected the instruments. Per hospital protocol was brought in fluoroscopy we identified the metal fragment the posterior compartment of the knee. Was initially localized in the soft tissue the posterior aspect of the knee where I attempt to retrieve using anterior portals under direct visualization, then had to use the arthroscopy specifically a 70 degree scope posterior portal. Then made an accessory posterior medial portal and was able to excise the metal fragment. Used fluoroscopy to confirm fragment removal and notified the patient in the recovery room.
We did a root cause analysis for this complication and felt 1 contributing factor to improve upon is to ensure an ACL reconstructions revision where there may be previous tunnels to ensure we start the drill tip prior to contact with the bone. Moreover we are creating a standardization of reviewing instruments at th preoperatively the patient was consented for a block e completion of the case much like we do a needle and sponge.

However given the fact that it was not guaranteed ACL reconstruction we decided to wait to assess postoperatively. He elected to not undergo block after surgery.
In the operating room once the patient was put to sleep under anesthesia performed a Lachman pivot shift. There were positive and made a decision to proceed with an ACL reconstruction. In addition this was confirmed with direct visualization where I saw the generally lax ACL under direct visualization and palpation.
In addition identified lateral compartment chondrosis which I debrided as well as a small posterior medial meniscal tear which I debrided as well. That the diagnostic arthroscopy did not yield any other significant findings

Once I debrided the ACL remnant off of the femoral condyle placed the Arthrex the scope in the medial part of the portal to better visualize tunnel location. I can see that the previous tunnel was so vertical that I was able to either use a flip cutter or anterior medial portal to anatomically reconstruct the femoral tunnel during the revision not have interference with the previous tunnel. Objectively much more comfortable with anterior medial portal low-profile reamer as opposed to the flip cutter site so I chose to use this technique.

After placing the new tunnel is generally satisfied with my tunnel placement as well as a confirmed procedure well integrity, integrity from previous tunnel and I passed a Beath pin for suture.
I was able to use the same tunnel on the tibia where the past 11 mm cigar reamer over the Beath pin. I was able to keep the previous screw in place is that there was bone overgrowth and it did not interfere with the second interference metal screw fixation it actually enhanced fixation why do not feel I need to have any backup.

Here are final pictures of the graft in flexion and extension. Postop physical examination was 1 a Lachman with a firm endpoint. Duration of surgery was 1 hr 35 minutes with 25cc estimated blood loss.
Patient was discharged with multimodal pain meds, limited narcotics, aspirin and ice/crutches, WBAT in Bledsoe brace with routine ACL protocol
2/6W routine
3 month telemedicine
9 months return to sport.

Patient general postop course was uncomplicated for the first 6 weeks. Then COVID hit and his 3 month follow-up was performed via telemedicine. I saw him at 2 weeks, 6 weeks, 3 months and 9 months which is mostly consistent with my routine recovery program.
My last follow-up visit was approximately 9 months status post surgery and he is generally doing well.