CNS 5 (Oct 8) Flashcards
(43 cards)
When you see someone crying, what response is activated?
-empathetic response is activated in the amygdala
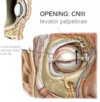
What muscle opens the eyelid? What nerve is it innervated by?
- levator palpebrae
- CN III
What muscle is repsonsible for creating facial expressions by closing the eye?
- orbicularis oculi
- innervated by CN VII
- blinking happens automatically through this sytem and voluntarily

What are saccadic eye movements?
- necessary for fovea to be exposed to the entire scene
- muscles need to be able to move around within the orbit to be able to scan
What purpose do the oblique muscles in the eye serve?

-correct movements of eye up and down (rectus muscles do not go straight back)

How is eye adducted and abducted?
- contraction of lateral rectus (CN VI) and medial rectus (CNIII) muscles
- abduct: lateral, adduct: medial
What two muscles work together to get movement of eye directly upwards?
- superior rectus will pull eye up and outwards (laterally)
- inferior oblique will pull eye up and inwards (medially)

What two muscles work together to get movement of eye downwards?
- inferior rectus pulls eye outwards and downwards (CNIII)
- superior oblique pulls eye downwards and inwards (CNIV)

What causes diplopia?
- diplopia=double vision
- overstretched extraocular muscles or probelm with innervation left and right eye can sometimes not work together properly (conjugate eye movements)
Where is the lesion?

- eye is in abducted position indicating abducens nerve is working properly
- CNIII is paralyzed so eye is pulled outwards
- oculomotor palsy
Where is the lesion?

- trochlear palsy
- CNIV innervates the superior oblique muscle
- patients with CNIV palsy complain of double vision especially when going downstairs, double vision looking downwards, and even though they have been corrected for optical error they still have difficulty reading
- can test by tilting the head and see that one eye has abnormal movement
Where is the lesion?

-abducens palsy
- CN VI
- supplies lateral rectus muscle
-CNIII innervating medial rectus muscle is contracting and is unopposed and as a result the eye is pulled nasally
What is happening with patient A?

- patient asked to follow the pencil
- eye is in abducted position
- lesion is in CNIII
- abducens nerve is pulling the eye to the side and is also accompanied with a ptosis
What is happening with patient B?

- ask patient to fixate on pencil
- right eye is paralyzed
- medial rectus muscle on the left eye is working properly but they can’t look to the side with the right eye
- CNVI which is innervating the lateral rectus muscle
Which structure controls lateral gaze?
- PPRF
- paramedian pontine reticular formation
- located in pons
Describe the process of lateral conjugate eye movements
- Frontal eye field will inform the PPRF that your eyes need to move to the side (ex: want to move eye to the left, info will go into left PPRF)
- This causes stimulation of abducens nucleus (L in this example)
- Left lateral muscle contracts (innervated by CNVI)
- At the same time, the PPRF sends message along the left medial longitudinal fasciculus
- This crosses over and innervates the CNIII on the right side (right oculomotor nucleus)
- Causes right medial rectus muscle to contract and move to the left as well

Describe the system to see things close up
- convergence and accomodation system
1. optic nerve sees object and projects to the superior colliculus
2. Superior colliculus sends impulse into CNIII nucleus which causes both medial rectus muscles to contract and converges the eyes to focus on the object
3. CNIII is closely associated with neurons that constrict the pupil and contraction of ciliary body muscle; parasympathetic innervation from the area around CNIII to the ciliary body and the pupil constricter
4. When ciliary body is constricted, it allows lens to round up and magnify
5. Pupillary constricter closes to increase the depth of field of the eye

How does ciliary body muscle contraction affect the lens?
- normally lens is flat and stretched
- ciliary muscle contracts and pulls everything to the front
- smaller distance at front of the eye so as it’s pulled towards the front, the fibres that attach the lens to the sclera now become more relaxed
- lens becomes relaxed and more round
- goes up several diopters

What makes the iris so opaque?
- pigmented iris epithelium
- very dense black pigment at back of eye
- even in blue eyed person who has no pigment in the stroma of the eye, it is just as effective because everyone (except albino) has the pigment layer lining back of iris
Describe pupillary sphincter and pupillary dilator muscles
sphincter: runs around the iris so when it is constricted the pupil gets smaller
dilator: runs along the length of the iris and it pulls the tip of the iris apart to widen the pupil

Describe parasympathetic pupil control
- preganglionic neuron starts in midbrain then follows along the CNIII until it reaches the ciliary ganglion
- synapses at ganglion then postganglionic nerves causes pupillary constriction

Describe sympathetic pupil control
- begins in thorax
- link between lateral horn of the spinal cord and the hypothalamus where sympathetic nerves are located
- preganglionic nerves to the eye have to enter the sympathetic trunk
- synapse in the ganglion at the top of the neck: superior cervical ganglion
- postganglionic nerves get on carotid artery and follow it along the BVs that go into the eye and innervate pupillary dilator

What is Horner’s syndrome?
- sympathetic lesion
- eye droop (ptosis)
- eyelid has two muscles: skeletal muscle that voluntary opens the eye and smooth muscle that keeps the eye open in sympathetic response (drooping of eyelid when that muscle is lesioned)
- miosis
- anhydrosis
- hyperemia (flushed skin)
What is happening to patient A?

- pupil is dilated
- mydriasis
- possibly lesion of CNIII parasympathetic fibres
- also could be drug use, sex, stroke








