RESP2 Flashcards
(55 cards)
What are the types of primary lung cancer?
- Non small cell - adeno, squamous and large cell
adeno is most common
Non small cell is less aggressive
- Small cell - rarer and more aggressive
Management of lung cancer
Depends on histology
Small cell - poorly diferentiated
- usually not appropriate for curative surgery b/c there’s spread at diagnosis.
Chemo is possible - but only extends life 3 months to 1.5 years
NON small cell - adeno/sq/large -
Curative resection is the aim
Radiotherapy is mostly palliative
What is bronchiectasis?
Morphologically - Permanent dilatation of bronchi and bronchioles
Clinically - Chronic cough, Recurrent or persistent bronchial infections AND often discoloured sputum production
Pathophys - small airway bronchiolitis –> protease production –> causes damage to large airways –> permanent dilatation
– MILD TO MODERATE OBSTRUCTIVE AIRWAYS DISEASE
What is a traction bronchiectasis?
In an area of lung fibrosis
Traction effect from fibrosis of adjacent bronchioles causes dilatation.
What are the risk factors for development/causes of bronchiectasis?
- Broncial obstruction - foreign bodies, impaction of mucous, atopic asthma, chronic bronchitis, tumour
-
Congenital or hereditary conditions
- cystic fibrosis - abnormally thick mucous
Immune deficiency states
Kartagener syndrome - situs inversitus, bronchiectasis, Sinusitis
- Necrotising or Supprative Pneumonia - often Staph species or Klebsiella, Mycobacterium Avium Complex, Aspergillus Fumigatus
- Mucocillary defects - Primary Cillary Dyskinesia
- Autoimmune conditions - Rheumatoid
Patient with symptoms of persistent chest infection, not responding to treatment and Pseudomonas Aeruginosa (or other gram negative) is found on culture. Which diagnosis must be excluded?
Bronchiectasis
Clinical Features of Bronchiectasis?
Dyspnoea, chronic cough, sputum, haemoptysis, malnutrition/LOW
Mild disease - symptoms with chest infections
Severe disease - recurrent febrile episodes with pneumonia, chronic COP (copious, offensive, purulent) sputum, LOW, LOA, Finger clubbing in 5%, haemoptysis
o/e
Finger clubbing 5%
central trachea
reduced chest expansion
Can have creps and rhonchi - bi basal creps common
When would you start antibiotics in an exacerbation of bronchiectasis?
MUST HAVE ALL THREE
- Increased sputum volume
- increase purulence
- Increased COUGH
Patient presents with years of chronic cough and sputum production - discoloured sputum. Bibasal crepitations on examination. Diagnostic investigation?
HRCT
In cross section - Internal calibre of the bronchus is larger than the adjacent pulmonary vessel (Arterial branch) - Signet ring sign
IN longitudinal - Failure of bronchi to taper
Investigations in suspected bronchiectasis?
HRCT
Sputum test M/C/S and acid fast bacilli
FBE, LFT, UEC
Spirometry
Special diagnostic tests for associated conditions- eg sweat testing in kids for CF,
RF and ANA, Immunoglobulin concentrations (IgE, IgA, IgM, IgG)
Aspergillus serology
What is your management approach for a patient with bronchiectasis?
Management should be individualised in collaboration with a respiratory physician with a specific treatment plan.
- Prompt treatment of exacerbations.
- Avoid infections - sick kids, babysitting, sick contacts,
- Clear the airway of sputum - Chest physiotherapy
- Routine Vaccinations for Influenza and pneumococcal coverage
- Regular Review - annual in adults, 6 monthly in kids - at this time sputum culture/check for complications/disease progression and severity
Which subset of bronchiectasis is rapidly progressive
Likely those who are colonised by pseudomonas
Which antibiotics would you use for a bronchiectasis exac?
For non pseudom - same as CAP
Amox 1g TDS
or
Doxy 100mg bd
If recent Haemoph Inf or Moraxella
Augmentin DF (Amox and clavulanic acid 875 + 125 - one bd
If pseudo
Cipro 500mg bd
Which pathogens are associated with exacerbations of Bronchiectasis
Haemophillus influenzae
Strep Pneumo
Moraxella
Pseudomonas - if present - repeat the culutre and discuss with specialist - as this can be rapidly progressive
What are the clinical features of bronchiolitis?
- wheeze
- fever
- Cough
- Coryza
- tachypnoea
- +/- work of breathing/
- +/- feeding difficulties
- o/e widespread wheeze and crackles
- Infant under 12 months
Infectious agent in bronchiolitis
RSV
or rhino
Priniciples of management
Supportive
Support oxygenation and feeding
no ix or abx
Risk factors for more serious illness
Age less than 10 weeks at presentation
Chronic lung disease
Chronic neurological
Downs Syndrome
Indigenous ethnicity
Immune compromise
Admission criteria for bronchiolitis?
Moderate to severe work of breathing - RR, tracheal tug, nasal flaring, recessions
Oxygen saturations less than 94%
Feeding problems
Tachypnea RR
Further managment of Bronchiolitis?
O2 therapy only if sats persistently below 90%
Small frequent feeds
If clinically dehydrated - may need NG feeds or IV
Parental education (Handout from the RCH on bronchiolitis)
Complications of Bronchiolitis
Dehydration from feeding issues
Hypoxaemia
Bronchiolitis Obliterans (Can lead to permanent lung damage)
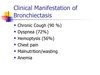
What are the clinical features of Bronchial Cancer?
1. Respiratory
Cough - over three weeks needs CXR
- SOB - exertional - can be due to lobar collapse or underlying lung disease
Wheeze
Prolonged/unresolving chest infection
Chest pain - central dull if mediastinal mass or node invasion, peripheral sharp if pleural/chest wall invasion
- Local spread- PanCoast tumour - apical lung - Invasion symapthetic trunk - horners, Invasion of C8/T1 - and brachial plexus - pain in upper limb and wasting of small muscles of hand (+/- 2nd rib pain)
- Constitutional symptoms
LOA, LOW
- Metastatic symptoms
Brain -H/ache
Liver - LOA, LOW
Bone - #
Adrenal - usu asympto
Investigations for broncial cancer?
CXR - can miss it sometimes ( A solitary nodule - granuloma, harmartoma, bronchial adenoma)
CT - if done for staging needs to include the abdomen
A LN less than 1cm is not considered enlarged but can still have cancer cells.
PET/CT - investigation of choice for staging
Fibreoptic bronchoscopy ( another type is fluorescence bronc can detect premalignant cells)
Endobronchial USS and biopsy, also u/s guided biopsy of supraclavicular lymph node can be done.



