Pathoma Pulm Flashcards
Nasal Polyp
- Protrusion of edematous, inflamed nasal mucosa
- Usually due to repeated bouts of rhinitis
- Occurs in CF and Aspirin-intolerant Asthma (triad of asthma, aspirin induced bronchospasms, and nasal polyps)

Angiofibroma
- Benign tumor of nasal mucosa composed of large blood vessels and fibrous tissue
- Classically seen with adolescent males
- Presents with diffuse epistaxis
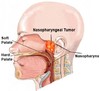
Nasopharyngeal Carcinoma
- Malignant tumor of the nasopharyngeal epithelium
- Associated with EBV, classically seen in African children and Chinese adults
- Pleomorphic keratin-positive epithelial cells in a background of lymphocytes
- Often involves cervical lymph nodes
Most common cause of acute epiglottitis and common X-ray finding
H. Infleunzae type B (esp in nonimmunized kids)
Presents with high fever, sore throat, drooling with dysphagia, muffled voice, and inspiratory stridor
- High risk of airway obstruction
- Thumb print sign

Laryngotracheobronchitis and a classic X-ray finding
=Croup
Parainfleunza virus is most common cause
- Presents with hoarse “barking” cough and inspiratory stridor
- Steeple sign

Broadly, three types of pneumonia and the sputum often seen
- Lobar pneumonia
- Bronchopneumonia
- Interstitial pneumonia
Usually see productive cough with yellow-green (pus) or rusty (blood) mucus
…also can see
- Aspiration Pneumonia
- TB

Lobar pneumonia
Consolidation of ENTIRE lobe of lung
usually bacterial
Two most common causes are:
- S. Aureus: most common cause of community acquired pneumonia and secondary pneumonia (often after infleunza)
- Klebsiella (enteric bacteria, must be aspirated from gut). Often accompanied by abscess
4 phases of lobar pneumonia
1. Congestion: congested vessels and edema
2. Red hepatization: due to exudate, neutrophils, and hemorrhage filling alvbeolar air spaces
3. Gray hepatization: due to degredation of red cells within exudate
4. Resolution: heal by resolution via Type II pneumocytes (regenerate BOTH type I and type II, the stem cells of the lung)
Bronchopneumonia
-Scattered patchy consolidation centered around bronchioles, often multifocal and bilateral
Caused by:
- Staph Aureus: 2nd most common cause secondary pneumonia
- H. Infleunza: common superimposed on COPD
- Pseudamonas: common CF pts
- Moraxella: CAP and COPD
- Legionella: CAP, COPD, or immunocpmpromised or water source (remember silver stain)
Interstitial (atypical) pneumonia
- Diffuse interstitial infiltrates
- Present with relatively mild URI sx (minimal sputum and low fever)
Caused by:
- Mycoplasma pneumonia: most common cause, young adults. Autoimmune Hemolytic Anemia common (IgM against I antigen on RBC; cold agglutinin)
- Chlamydia pneumoniae: 2nd most common
- RSV: most common in infants
- CMV: common in post-transplant pts
- Influenza Virus: elderly, immunocompromised. Increased risk of secondary
- Coxiella Burnetii: Q fever seen in farmers/vets (spores by ticks on animals). This is rickettsial organism but NO RASH, NO ARTHROPOD (spore)
Aspiration pneumonia
- seen in pts at risk for aspiration: alcoholics, comatose pts
- Anaerobic bacteria (bacteroides, fusobacterium, peptoccus)
Basic principles of COPD
-Problem getting air OUT
Decreased FVC, Decreased even more FEV1 resulting in a decreased FEV1:FVC ratio (think if normal was 5L and you could do 4L in first second, ratio would be 4/5=80%. Here we see more of a decrease in first second so we are down to 2 and total decrease to 4 so 2/4=50%
-TLC is usually increased due to air trapping
Chronic Bronchitis pathophys
- Cough lasting 3 months over minimum 2 years
- Highly associated with smoking
- See hypertrophy of bronchial mucinous glands (leading to thickness of mucus glands relative to bronchial wall tickness = Reid Index. >50% seen in bronchitis, <40% normal.
Pink Puffer vs Blue Bloater…what is each associated with and why
Blue Bloater: Chronic Bronchitis. Mucus plugs trap CO2 and if have an increase in PCO2, then will decrease PAO2 (alveolar) and thus decrease PaO2 (arterial) and result in cyanosis.
Pink Puffer: Emphysema. Due to prolonged inspiration with pursed lips in an attempt to create back pressure and stop the walls from collapsing in on themselves. They are getting enough air but it takes a LOT of work, so they are skinny as shit. Also have barrel chest

Emphysema pathophys
- Destruction of the alveolar air sacs. Loss of elastic recoil and collapse of airways during exhalation results in obstruction and air trapping.
- Due to an imbalance of proteases and antiproteases
1. Increase in proteases seen in SMOKERS, due to excessive inflammation and release of proteases by neutrophils and macrophages
2. Decrease in antiproteases seen in Alpha1-antitrypsin deficiency (meant to neutralize protease). This also presents as liver cirrhosis as these are made in liver and are misfolded and stick around in ER of hepatocytes and wreck havoc (PAS+ stain in hepatocytes)

Panacinar vs Centriacinar emphysema
Centriacinar: caused by smoking. Most severe in upper lobes (smoke rises, and smoke hits center of all tubes in lungs)
Panacinar: seen in alpha1 antitrypsin deficiency. Most severe in lower lobes

Asthma pathophys
- Reversible airway broncoconstriction due to allergic stimuli
- Type 1 Hypersensitivity. Allergens induce TH2 cells to secrete IL-4 (mediate class switch plasma –>IgE), IL-5 (eosinophils), and IL-10 (stimulate TH2 and inhibit TH1)
Asthma reexposure to allergen leads to…
-IgE mediated activation of MAST CELLS
- release preformed histamine granules and generation of leukotrienes C4, D4, E4 lead to bronchoconstriction, inflmamation, and edema (early phase reaction)
- Inflammation, especially major basic protein dereived from eosinophils damages cells (late phase reaction)
Asthma pathology
Spiral shaped mucus plugs (curschmann spirals) and eosinophil-derived crystals
-Charcot-leyden crystals present

Bronchiectasis
Permanent Dilation of bronchioles and bronchi (loss of airway tone) resulting in air trapping (think blowing through big pipe)
-Can result in cor pulmonale and secondary AA amyloidosis
Causes:
- CF
- Kartagener syndrome (defect in dynein arm, which is necessary for ciliary movement)
- Tumor or foreign body
- Allergic bronchipulmonary aspergillosis: hypersensitivity reaction to aspergillus leads to chronic inflammatory damage, usually seen in individuals with asthma or CF
Basic principle of Restrictive Lung Diseases
-Decreased TLC
Decreased FEV1 but MORE decrease FVC (so if lung capacity was VC was 5L and 4 out on first second, would be 4/5=80%. Here we have decreased FEV1 a little to 3.5 and decreased FVC to 4 so see >80%
-Most commonly associated with interstitial diseases of the lung but can also present due to obesity or neuromuscular issues
Idiopathic Pulmonary Fibrosis
- Fibrosis of lung interstitium Likely related to cyclical lung injury. TGF-B from injured pneumocytes induces fibrosis
- Need to exclude secondary causes such as bleomycin, amiodarone, radiation therapy
Tx: lung transplant


















