Pathoma Renal Flashcards
Horseshoe Kidney
-Conjoined kideny connected at lower pole. Most common congenital renal anomaly.
Gets caught on Inferior Mesenteric Artery during its ascent, so STAYS in inferior abdomen
- This kidney (just one since the two are fused), functions normally
- Associated with hydronephrosis, renal stones, infection, chromosome aneuploidy syndromes (Turner, 13, 18, 21)

Renal agenesis (two types)
-Unilateral agenesis: leads to hypertrophy of existing kidney, hyperfiltration leads to increased risk of renal failure later in life (uteric bud fails to develop and induce differentiation of metanephric mesenchyme)
-Bilateral agenesis: leads to oligohydramnios with lung hypoplasia, flat face, low set ears, developmental defects in extremities (Potter Sequence). Incompatible with life
Multicystic Dysplastic Kidney
- Ureteric bud fails to induce differentiation of metanephric mesenchyme –> nonfunctional kidney
- This is NOT inherited (unlike PKD), if bilateral, must differentiate between this and PKD.
- Usually the cysts consist of connective tissue such as cartilage.
Two types of Polycystic Kidney Disease
1. Autosomal Dominant in ADults: presents as HTN (due to increased Renin), hematuria, and worsening renal failure. ALWAYS bilateral. Progress to renal failure in 50% pts. Mutations in PKD1, chr 16 (85%) and PKD2, chr 4 (15%). Associated with Berry Aneurysms (cause of death), Mitral Valve Prolapse, Benign Hepatic Cysts Tx: ACE-I, ARB
2. Autosomal Resessive: presents in infants as worsening renal failure and hypertension. Newborns present with Potter Sequence. Cystic dilation of collecting ducts. Presents like portal HTN (due to hepatic cysts, associated with hepatic fibrosis
Medullary Cystic Kidney Disease
-AD defect leading to cysts in the medullary collecting ducts
Results in SHRUNKEN kidneys and worsening RENAL FAILURE
-Poor prognosis
Azotemia
-Increased BUN and Creatinine (high levels of nitrogen containing compounds)
Pre-renal azotemia
- Due to decreased renal blood flow (cardiac failure)
- This results in decreased GFR, azotemia, and oliguria (decreased urine)
- BUN:CR >15, FENa <1% (nothing wrong with tubules themselves, just getting less to work with.

Post-renal Azotemia
- Due to obstruction of urinary tract downstream from the kidney (stones, BPH, neoplasia, congenital anomalies) Develops only with BILATERAL obstruction
- Results in decreased GFR, azotemia, oliguria
1. EARLY stage: increased tubular pressure forces BUM into blood so BUN:CR >15, FENa still intact so <1% and urine osm >500
2. LONG-STANDING obstruction: tubular damage ensues, resulting in decreased reabsorption of BUN (BUN:CR<15), decreaed reabsorption of Na FENa >2%, inability to concentrate urine (urine osm <350)

Acute Tubular Nectosis overview
- Injury and necrosis of tubular epithelial cells (most common cause of acute renal failure that is intrarenal azotemia)
- These necrotic cells plug tubules (obstruction decreases GRF). Brown, granular casts are seen in the urine.
- Since the tubular epithelium is dysfunctional, decreased reabsorption of BUN (BUN:Cr <15), decreased reabsorption of sodium (FENa >2%), and inability to concentrate urine (<350)
Acute tubular necrosis types (2)
1. Ischemia: often preceeded by prerena azotemia (hypotension, shock, sepsis, hemorrhage, CHF). Results in death of tubular cells that slough into tubular lumen, PCT and Thick Asc Limb are affected
2. Nephrotoxic: toxic agents result in necrosis of tubules. Aminoglycosides (most common), Heavy metals (lead), myoglobinuria (crush injury), ethylene glycol (oxalate crystals in urine), radiocontrast dye, urate (tumor lysis syndrome –> give allopurinol and hydration prior to chemo to decrease risk of urate-induced ATN). PCT susceptible to injury
Acute Interstitial Nephritis
-Drug-induced hypersensitivity involving interstitium and tubules resulting in acute renal failure (tubules are fine, it is interstitium that is affected)
(INTRARENAL AZOTEMIA)
-Classically see eosinophils** (diagnostic)
Causes are P’s
Pee (diuretics)
Pain-free (NSAIDS)
PCN and Cephalosporins
PPI
RifamPin
Acute Interstitial Nephritis key findings
- Muddy brown casts (grannular)
- Eosinophils are hallmark cell
- Hyperkalemia, metabolic acidosis, uremia

Nephrotic Syndrome basic overview and 6 types
Proteinuria >3.5 g/day
Results in hypoalbuminemia (pitting edema), Hypogammaglobulinemia (increased risk infection), Hypercoagulable state (loss antithrombin III), Hyperlipidemia and hypercholesterolemia (blood is so thin that liver dumps more into it)
1. Minimal Change Disease
2. Focal Segmental Glomerulosclerosis
3. Membranous Nephropathy
4. Membranoproliferative Glomerulonephritis
5. Diabetes Mellitus
6. Systemic Amyloidosis
Most common Nephrotic Syndromes in these pt groups
- Children
- Hispanics and African Americans
- Caucasian Adults
- HBV/HCV pts
- HIV, heroin use, Sickle Cell disease
- Solid tumors, SLE, NSAIDS, Penicillamine
- Children –> MCD
- Hispanics and African Americans–> FSGS
- Caucasian Adults –> Membranous Nephropathy
- HBV/HCV pts –> Membranoproliferative Glomerulonephritis (type 1), OR Membranous Nephropathy
- HIV, heroin use, SIckle Cell Disease –> FSGS
- Solid tumors, SLE, NSAIDS, Penicillamine –> Membranous Nephropathy
Minimal Change Disease
- Most common nephrotic in children
- May be associated with Hodgkin Lymphoma
- Normal H&E stain. Effacement of foot processes on electron microscopy
- NO immune complex deposits (Negative IF)
- Selective proteinuria (loss of albumin, but not immunoglobulin)
- Excellent response to steroids (damage mediated by cytokines from T cells)

Focal Segmental Glomerulosclerosis (FSGS)
- Most common cause of nephrotic syndrome in Hispanics and AA.
- Associated with HIV, Heroin use, Sickle Cell
- LM:segmental sclerosis and hyalinosis
EM: Effacement of foot processes
-IF: Negative
Poor response to steroids, progress to renal failure
Membranous Nephropathy
- Most common cause of nephrotic syndrome in Caucasian adults
- Associated with Hep B, C, solid tumors, SLE, drugs (NSAID, Penicillamine)
- LM: THICK glomerular BM
IF: granular,
EM: subepithelial deposits with DOME AND SPIKE

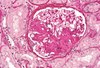
Membranoproliferative Glomerulonephritis
-CAN BE CONSIDERED NEPHRITIC OR NEPHROTIC
-mesangial cell proliferation of cytoplasm is what creates the tram track appearance (trying to encorporate the immune complex depositon)
LM: thick glom BM with TRAM-TRACK appearance
- IF: immune complex deposition
- Two types
1. Type 1: subendothelial. Associated with HBV, HCV, increased Tram tracking
2. Type 2: intramembranous. Associated with C3 nephritic factor (autoantibody that stabilizes C3 convertase leading to overactivation of complement)

Diabetes Mellitus in context of nephrotic disease
- High glucose –> nonenzymatic glycosylation of vascular BM resulting in hyaline arteriolosclerosis
- Efferent arteriole >Afferent leading to high glom filtration pressure –> microalbuminuria -> nephrotic syndrome
Characterized by Kimmelsteil-Wilson nodules (sclerosis of the mesangium)
Tx: ACE-I slow progression













