Fractures Flashcards
(18 cards)
What is more importnat in preventing osteoporosis? Structure or composition of bone?
Structure is more important
How is osteoporosis assessed?
Assessed using DEXA scans:
- T score – based off score of a white pre-menopausal woman.
- Z score – age and gender matched score.
* Range is -4.0 –> +1.0 (osteoporosis = <-2.5).
What are the main 4 cells involved in bone turnover?
- Osteoclasts – break down bone – big and have a ruffled border.
- Osteoblasts – lay down new bone.
- Osteocytes – mature osteoblasts – act as mechanoreceptors.
- Osteoprogenitors.
- Normal bone turnover is continuous – 5% at any one time.
- Osteoclast ruffled borders contain the digestive bone enzymes.
- Bisphosphonates destroy the osteoclast cytoskeleton which breaks down the ruffled border so they no longer can release digestive enzymes.

How do bisphosphonates work? What are the bad effects of bisposphonates?
Bisphosphonates destroy the osteoclast cytoskeleton which breaks down the ruffled border so they no longer can release digestive enzymes.
Bisphosphonates inhibit the constant bone remodelling (so limit the bone reabsorption) but this can lead to a build-up of microfractures which can then spontaneously break over time and use.
- Supressed activity can make bones MORE brittle (the exact thing bisphosphonates try to stop).
- Fractures – atypical fractures – typically sub-trochanteric.
What are the steps involved in bone remodelling?
Activation occurs when there is damage or hormonal activation –> increased expression of RANKL –> osteoclast activation
The remodeling cycle consists of three consecutive phases:
- resorption, during which osteoclasts digest old bone within a sealed resorption vacuole - (release of factors from bone matrix recruits osteoblasts) Once accomplished their function, osteoclasts undergo apoptosis.
- reversal, when mononuclear cells appear on the bone surface(which probably remove debris from matrix degradation); preosteoblasts
- formation, (stored GF are released and recruit osteoblasts) osteoblasts lay down new bone until the resorbed bone is completely replaced. Initially not calcified (oseoid) then mineralisation occurs with hydroxyapatite.

Describe the MOA of denosumab.
Denosumab – OPG analogue / RANK analogue- suppresses bone resorption markers (RANKL is the primary signal to promote removal/resorption of bone)
Denosumab prevents RANKL from activating its receptor RANK on the surface of osteoclasts
Osteoclasts – exhibit RANK.
Osteoblasts – exhibit RANKL.
OPG also acts to supress osteoclast activation.

How does exercise affect bone strength?
Wolff’s Law – the bone remodels according to the stresses applied to it – e.g. exercise.
Internal structures of trabeculae undergo adaptive changes whilst secondary appositional bone growth can occur.
- Type of exercise matters too e.g. deep flexion best for neck of the femur.
- This is important to consider in healing patients.
- There is a need for exercise and a healthy diet in the younger population so that we can build up sufficient “stores” for so we can lose more before osteporosis
- Note that it is not just exercise that influences bone growth but also diet, VitD, PTH, calcitonin, etc.
What hormones are involved in calcium homeostasis?
· Vitamin D
· Calcitonin
· PTH/Calcitriol
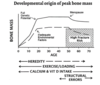
How does bone mass change with age? Why is this important?
- Bone mass increases until peak bone mass in late teens
- Stays relatively steady until menopause
- Decreases rapidly after menopause
Importance:
Bone mass cannot reach its peak genetic potential without adequate environmental factors such as good diet and exercise
What are the 4 stages of fracture healing?
- Haematoma/inflammation - up to 1 week
- Soft callus formation - 1-4weeks
- Hard callus formation - 1-4months
- Remodelling - up to several years.

Describe the first stage of fracture healing.
Stage 1 – Haematoma/Inflammation – up-to 1 week.
- Macrophages, leucocytes, IL-1-6, BMPs.
- Granulation tissue formation.
- Progenitor cell invasion.
Describe the second stage of fracture healing.
Stage 2 – Soft callus formation – 1-4 weeks.
- Chondroblasts –> collagen II; fibroblasts –> fibrous tissue.
- Proteoglycans produced (prevent mineralisation).
- Chondrocytes release calcium + enzymes to break down proteoglycans (allows mineralisation).
Describe the third stage of fracture healing.
- Stage 3 – Hard callus formation – 1-4 months.
- Blood vessel invasion of soft callus.
- Chondroclasts break down calcified callus and this is replaced by osteoid (Type I collagen) from osteoblasts.
- Osteoid calcified into WOVEN bone (which is not very organised)
Describe the fourth stage of fracture healing.
- Stage 4 – Remodelling – up-to several years.
- Woven –> lamellar bone (trabeculae become aligned)
- Shapes according to Wolff’s law/relative to stresses
- Medullary canals form again
What is preferred: completely stable or flexible fixation of fractures?
When the bone is completely stable, without movement, the bone heals in a straight line with little callus – this is primary bone healing
Osteoclasts cut away at the damaged bone and osteoblasts lay down new bone – cutting cone mechanism
Secondary bone healing – can be seen in flexible fixation of fractures, such as fractures stabilised by rods and casts – there is more callus
Secondary bone healing can go back to normal (decreased callus) in children very easily – due to increased bone remodelling
Are fractures and breaks the same thing?
Yes because both cortices are still crossed.
What is a greenstick fracture?
Occurs in toddlers
Cortex broken on only one side but not the other because of the flexibility of the bone
- Early callus seen at 7 days – becomes ossified so you can see it on X-ray
- Completely ossified – woven bone at 2 weeks
- 6-12 months the bone becomes almost straight again – this is not the same in adults as healing isn’t as good.

Name the different types of fracture. Describe each.

- General fractures – left –> right of picture:
- Spiral fracture - due to rotational force
- Oblique fracture - crush injury
- Butterfly fragment fracture/comminuted fracture – high impact/blunt force trauma with no withdrawal of force
- Transverse fracture - e.g. patellar fracture where quad contracts so hard that they pull the bone apart; e.g. olecranon fracture. Trauma followed by withdrawal
Named purely by compressive forces.


