Pathogenesis of Autoimmune Disease (Part 2) Flashcards
(42 cards)
What auto-antibody is associated with systemic vasculitis?
antinuclear cytoplasmic antibodies (ANCA)
What auto-antibody is associated with diffuse systemic sclerosis?
Anti-Scl-70 antibody (AKA antibodies to topoisomerase-1)
What auto-antibody is associated with limited systemic sclerosis?
Anti-centromere antibodies.
What auto-antibody is associated with dermato-/Polymiositis?
Anti-tRNA transferase antibodies e.g. histidyl transferase (also termed anti-Jo-1 antibodies)
What auto-antibodies are associated with Sjögren’s syndrome?
No unique antibodies but typically see
- Antinuclear antibodies - Anti-Ro and anti-La antibodies
- Rheumatoid factor
What auto-antibody is associated with mixed connective tissue disease?
Anti-U1-RNP antibodies
Which auto-antibody is epecific to lupus?
Anti-double stranded DNA antibodies (anti-dsDNA).
Specific for SLE and SERUM LEVEL of antibody correlates with disease activity.
What is the commonest auto-antibody found in lupus?
Atinuclear antibodies (ANA)
Describe the laboratory test used for testing for ANA in lupus. Is this diagnostic of SLE?
- Human cells are placed on a glass slide, immobilised and permeabilised so that anything can bind to them.
- Patient serum is then added and if it contains ANAs then these will bind the the cells.
- To tell whether ANAs have bound, you add a fluorescently labelled monoclonal antibody that binds to the ANA and you observe the pattern of attachment
ANAs are NOT diagnostic of SLE.

If the ANA test comes back as positive, what will the lab do further tests for?
If ANA is positive the clinical laboratory will perform further tests to determine which type of ANA it is – typically these include screening for:
- Anti-Ro
- Anti-La
- Anti-centromere
- Anti-Sm
- Anti-RNP
- Anti-ds-DNA antibodies
- Anti-Scl-70
Cytoplasmic antibodies include:
- Anti-tRNA synthetase antibodies
- Anti-ribosomal P antibodies
Name the 4 patterns of ANA binding which can be seen iin different conditions.
- Homogenous
- Speckled
- Nucleolar
- Fine Speckled
Which auto-antibody level SPECIFIC for lupus does not correlate with disease activity?
Anti-Sm antibody (antigen is ribonucleoprotein)
What is the antigen of Anti-Ro and Anti-La antibodies in SLE?
ribonucleoprotein
What conditions other than SLE are ANti-Ro and Anti-La antobodies associated with?
- Secondary Sjögren’s syndrome
- Neonatal lupus syndrome (transient rash in neonate, permanent heart block)
What condition other than SLE are anti-ribosomal P antibodies associated with?
Cerebral lupus
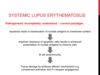
What is the current theory for the pathogenesis of systemic lupus erythematosus?
Which cells secrete these cytokines? What is their function?
- γ-IFN
- IL-1
- IL-2
- IL-6
- TNF-α

Describe the disease activity in SLE.
Sick lupus patient commonly has
- Low complement levels (complement is consmed by complexes when ill)
- High serum levels of anti-ds-DNA antibodies
What are the CD4+ T helper cell subsets?
Th1, Th2, Th17
What is TNF-a produced by and why is it called the dominant cytokine? Which inflammatory condition is it most associated with?
- It is produced by macrophages
- Inhibition of TNF-a results in blockage of production of IL-1, IL-8, chemokine IL-8 and GM-CSF therefore TNF-a is a DOMINANT cytokine
- It has pleotropic effects
- Dominant pro-inflammatory cytokine is the rheumatoid synovium

What is the function of Th1 cells?
Secrete IL-2 and γ-IFN and response is important in CD8 +ve cytotoxicity and macrophage stimulation
What is the fuction of Th2 cells?
secrete IL-4 (IgE responses), IL-5 (eosinophils), IL-6 (B cells to plasma cells) and IL-10 (inhibit macrophage response).
What is the function of Th17 cells?
- Develop in response to IL-23
- They secrete IL-17, a potent cytokine which triggers IL-6, IL-8, TNFα, matrix metalloproteinases and RANKL in target cells.
- Important in mucosal immunity but also in disease including arthritis, psoriasis, IBD and multiple sclerosis
Which cytokine causes inflammation of the synovium in rheumatoid arthritis?
TNF-alpha



