MBD - Histopathology Flashcards
(37 cards)
What is the role of bone biopsy in the diagnosis of metabolic bone disease?
- Confirm diagnosis of bone disorder find the cause of bone pain or tenderness
- Investigate abnormality seen on X-Ray
- Bone tumour diagnosis (benign vs malignant)
- Determine cause of unexplained infection
- Evaluate therapy performance
What are the types of bone biopsy?
- Closed- Jamshidi needle is inserted into bone and returns with a bone core sample
- Open- for sclerotic/inaccessible lesions e.g. in osteosclerosis or when a larger bone sample is required
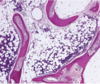
What type of bone samples is H&E staining used for?
Decalcified samples
What is Masson-Golder Trichome staining used for?
Looks at amount of mineralised vs unmineralised bone
Mineralised bone is coloured green and unmineralised osteoid recently produced is orange.
Useful in diagnosing osteomalacia.

What is tetracycline/Calcein labelling useful for?
Measure the rates of bone formation and turnover. Two injections given and distance between the two labels shows how much mineral accured between the two injections- this is the mineral apposition rate. Relationship between apposition rate and quantity of bone surface labelled tells the bone formation rate.
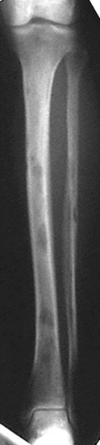
How mineralised does bone have to be to be seen on an X-Ray?
50%
What is a transilliac bone biopsy?
This is a typical location for non-bone specific bone biopsy. This allows a core sample with plenty of cortical and trabecular bone.
NB that type of bone sample seen on biopsy will depend on where it is taken from.
Name the types of anatomical bone.
Flat bones e.g.cranial bones, or ribs, which generally protect internal organs.
Long bones e.g femur and tibia, which support weight and facilitate movement
Short/cuboid bones e.g. carpals and tarsals, stabalise and facilitate movement
Irregular bones have a complex shape like the vertebrae or the pelvis. That allows them to protect a specific organ or set of organs.
Sesamoid bones like the patella found embedded in tendons which again have a protective function.
What are the differences between cortical and cancellous bone?
CORTICAL
- long bones
- 80% of skeleton
- appendicular
- 80-90% calcified
- mainly structural, mechanical, and protective
CANCELLOUS
- vertebrae & pelvis
- 20% of skeleton
- axial
- 15-25% calcified
- mainly metabolic
- large surface area
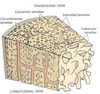
Name the microscopic structure types in bone.
Woven bone (immature) - lamellae absent, collagen fibres are disorganised
Lamellar bone (mature)
Describe the microanatomy of bone
- Cortical bone is made of parallel osteons
- Osteons are 0.2mm in diameter
- They have a central canal in the middle called the Haverisan canal which contains veins, arteries and a mechanosensory network
- Circumferential lamellae surround the whole bone at the periosteum
- Interstitial lamellae are found between the osteons
- Trabecular canals are organised in layers
What is the function of osteocytes?
Mechanosensory network embedded in mature bone. Make up >90% of bone cells
How do osteoblasts regulate the activity of osteoclasts?
Osteoblasts regulate osteoclast formation and activity by producing the key osteoclast factors:
- RANK ligand
- M-CSF
- RANKL decoy receptor OPG.
List some common metabolic bone diseases.
- Osteoporosis
- Osteomalacia/Rickets
- Primary hyperparathyroidism
- Renal osteodystrophy
- Paget’s disease
What are the types of osteoporosis and their causes?
1º
- age, post-menopause - related or due to the rapid loss of bone mass that occurs in the 5 to 7 years following the menopause and there is no other pathological cause
2º
- drugs, systemic disease (including nutritional deficits, certain drugs, genetic conditions, and of course endocrine or metabolic disorders)
What is high turnover vs low turnover osteoporosis?
High turnover - both formation and resorption are increased but resorption is increased above level of formation
Low turnover - both are decreased but formation is decreased to a greater extent.
Describe the pathology of osteoporosis.
Imbalance in bone remodelling so more resorption than formation. Affects trabecular bone as it is more metabolically active.
Holes where the trabecular bone has been resorbed away and remaining trabecular bone is thinner and less interconnected
Cortical bone will become thin too -> compression fractures of spine, long impact fragility fractures in long bones.

What staining is useful for osteoporotic bone?
Normal staining - trabeculae will be thinner, fewer, free-floating (disconnected from any other bone). Regular histology doesn’t distinguish between high and low turnover.
Histomorphometic studies/tetracycline labellling - large amount of unmineralised osteoid in orange due to increased osteoclast activity.
However serum markers may be easier to interpret.
What are the two types of osteomalacia?
Deficiency of vitamin D - typically, causes hypocalcaemia
Deficiency of PO4 - phosphate wasting syndromes.
What are the histological features of bone in osteomalacia?
Osteoid produced by osteoblasts remains unmineralised (due to unsufficient calcium to form hydroxyapatite crystals) so orange on Masson-Trichrome stain.
What are the clinical features of osteomalacia?
- Bone pain/tenderness
- Fracture
- Proximal weakness
- Bone deformity
What is osteitis fibrosa cystica?
Resorption of bone and replacement with fibrous tissue and the formation of cysts like ‘brown tumours.

What is the difference between primary and secondary hyperparathyroidism?
1º -
- parathyroid adenoma (85-90%)
- chief cell hyperplasia
2º -
- chronic renal deficiency
- vit D deficiency
What are the histological features of hyperparathyroidism?
Classic tunneling resorption as osteoclasts penetrate the middle of the trabeculae and resorb a central canal.