Urticaria Flashcards
(38 cards)
What is urticaria?
Urticaria is a disease characterised by the development of wheals (also known as hives), angioedema or both.
What gender is more likely to get angioedema?
Women
What % of the population get urticaria?
20%
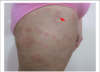
What are the 3 features of wheels?
- Pink or white raised areas of skin of variable size that resemble nettle stings
- They are usually itchy
- They have a fleeting nature with the skin returning to its normal appearance within 24 hours although the condition itself may last longer
What takes longer to resolve: angioedema or urticaria?
Angiooedema - it can take up to 72 hours to resolve.
What % of patients with urticaria will also get angioedema?
30%
What is the pathophysiology of urticaria?
- Degranulation of mast cell -> histamine & platelet activating factor release. -> Pruritus and vasodilation and increased permeability (leakiness) of blood vessels causing swelling and redness of the skin.
- Cutaneous nerves stimulation may release neuropeptides, either directly onto the blood vessel or via the mast cell, which can generate the wheal and flare urticated response.
Describe the Triple Response of Lewis.

- Red spot: due to capillary dilatation
- Flare: redness in the surrounding area due to arteriolar dilatation mediated by axon reflex
- Wheal: due to exudation of fluid from capillaries and venules
What are the 3 types of Urticaria?
- Acute spontaneous urticaria (ASU) < 6 weeks.
- Chronic spontaneous urticaria (CSU) > 6 weeks.
- Physical Urticaria
Aprt form length of time, what is the difference between ASU and CSU?
ASU usually has a trigger - Drugs, Antibiotics or Food.
CSU usually has no trigger.
What physical reactions occur in ASU and CSU?
Spontaneous wheels +/- angioedema.
In what age group does CSU occur in?
20-30 years.
What test can you do in ASU (acute spontaneous urticaria)?
RAST test or a Skin Prick Test
What are subtypes of physical urticaria?
- Dermographism
- Delayed Pressure urticaria
- Cholinergic urticaria
- Cold induced urticaria
- Solar urticaria
- Aquagenic urticaria
What is the main management for physical urticaria?
Avoid the physical trigger
Tell me about Dermographism

- 10% of population have it.
- Wheal lasts 30-60 mins.
- Symptomatic dermographism/factitious urticaria - severe cases of dermographism.
Tell me about delayed pressure urticaria
- Due to prolonged pressure to the skin.
- Clapping - causes the hands to swell
- Prolonged kissing - lips can swell.
*
Describe cholinergic urticaria.
- Micropapular urticaria that occursover the body after sweating.
- Not actually caused by acetylcholine but by neuropeptides released from nerve endings.
Describe cold urticaria
- Urticarial response after cold response.
- To diagnose:
- Put ice cube on skin
- The urticarial response will occur on Re-Warming the skin.
Describe solar urticaria
- Very rare
- Needs to be differentiated from polymorphic light eruption.
- Response is immediate.
- Light form the sun causes antigenic changes to proteins which mast cells then respond to by releasing histamine.
Describe Contact Urticaria
- Very common
- Usually due to contact with a foreign agent.
Describe the history taking
- Ask about the history of urticaria - where on the body, how long.
- Dietary history and correlation with food
- Medication history
- Allergy
- FH of atopy and urticaria
- Any concomitant medical history (e.g. bullous pemphigoid, SLE etc)
- Determine if angioedema+/- bronchospasm
- Recent infection or foreign travel.
In urticaria, what investigations should be done?
- Often no further invetigation is needed.
- Allergy avoidance
- RAST test or prick test can be organised.
- If CSU - no investigations are needed.
What conditions can mimic Chronic Spontaneous Urticaria (CSU)?
- SLE and other connective tissue diseases
- Bullous Pemphigoid and other immuno-bullous disorders
- Atopic eczema / pompholyx
- Thyroid dysfunction
- Contact dermatitis
- H.pylori gastritis
- Toxic erythema (especially drug reactions)
- Erythema multiforme
- Viral exanthema such as measles