Clinical Aspects of Pain Flashcards
What is the definition of pain?
How is it measured?
an unpleasant sensory and emotional experience associated with actual or potential tissue damange or described in terms of such damage
measurement is subjective
How is pain classified according to duration?
pain is either acute or chronic
What is acute pain associated with?
What type of pain is it usually?
What does it assist and resolve with?
associated with trauma or injury
usually nociceptive
- pain is proportional to magnitude of injury
- evolutionary protective function
- assists with wound healing
- resolves with healing
What is chronic pain?
What does it cause in the patient?
pain that persists past normal duration of tissue healing
(3 months)
may be dissociated from tissue damage
no obvious protective function and causes distress and suffering
What are the 3 pain classifications according to pathogenesis?
- nociceptive pain
- neuropathic pain
- psychogenic pain
What causes nociceptive pain?
it is caused by the presence of a painful stimulus on nociceptors
nociceptors in tissues send pain signals to the CNS
mechanisms involve endogenous opioids
What causes neuropathic pain?
it is initiated or caused by a primary lesion or dysfunction in the nervous system
damage to the nerve itself causes typical pain symptoms
it is often endogenous opioid independent
What causes psychogenic pain?
it is caused by the mental processes of the sufferer rather than by immediate physiological causes
What is the main difference between nociceptive and neuropathic pain?
What similarities do they have?
nociceptive pain:
- due to activation of nociceptors in tissues by a stimulus
neuropathic pain:
- due to damage to the nerve itself
both can be the underlying pathogenic mechanism for acute or chronic pain
both can appear together (e.g. back pain)

How is pain classified?
pain is multifactorial in nature
it can be primary nociceptive with injured/irritated somatic or visceral structure
it can be primary neuropathic with injury of a neural structure
it can have both nociceptive and neuropathic components

What are examples of primary nociceptive pain?
- osteoarthritis
- visceral pain
- headache
- ischaemic pain
- cancer pain / back pain (without nerve injury)
What are examples of primary neuropathic pain?
- peripheral back pain due to nerve injury
- trigeminal neuralgia
- HIV
- CRPS II
- phantom pain
- multiple sclerosis
- spinal cord injury
- post stroke
What are examples of pain including both a nociceptive and neuropathic component?
- chronic back pain
- nerve lesion / dysfunction
- nociceptive activation from ligaments, joints, muscles, tendons
- cancer pain with nerve infiltration
- CRPS I
- osteoporotic vertebral fracture
How is pain assessed?
What are the problems associated with this?
measuring absolute pain is a problem
pain is a construct:
- synthesis of several observations including intensity, quality, etc.
relative distress:
- e.g. acid reflux in healthy 42 yr old v. acid reflux in 42 yr old with strong family history of ischaemic heart disease
What are some factors associated with changes in pain perception?
- anxiety
- depressed effect
- gender - socialisation / gonadotrophins
- circadian variation
- climatic conditions
How is pain assessed in clinic usually?
it is self-reported by the patient using a visual analogue score
pain is assessed at rest and during movement

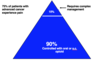
What is the adult acute pain intensity score?
a score of 0 - 3 that is used to assess pain intensity on movement

What is the natural history of acute nociceptive pain like?
How is it mediated?
the sensory experience of acute pain caused by a noxious stimulus is mediated by a specialised high-threshold sensory system - the nociceptive system

What are the beneficial consequences of acute pain?
- part of trauma response
- protective as it avoids further damage
- learning experience
What are the adverse consequences of acute pain?
- humanitarian issues
- cardiovascular issues
- respiratory compromise
- hypercoagulation
When should the WHO analgesia ladder be consulted?
in acute pain only
What are the 3 levels of the analgesia ladder?
- non-opioid +/- adjuvant
- pain persisting or increasing*
- opioid for mild to moderate pain + non-opioid +/- adjuvant
- pain persisting or increasing*
- opioid for moderate to severe pain + non-opioid +/- adjuvant

What types of analgesics are used at the first level of the analgesia ladder?
- acetaminophen
- aspirin
- NSAIDs
- COX-2 inhibitors
What type of analgesics are used at the second level of the analgesic ladder?
- codeine
- dihydrocodeine
- tramadol
What types of analgesics are used at the third and final stage of the analgesic ladder?
- morphine
- fentanyl
- hydromorphone
- buprenorphine
- methadone
How can nociceptive pain from tissue damage be subdivided?
somatic:
- affecting bones or soft tissues
visceral:
- affecting the gut and/or organs
What is the efficacy of NSAIDs like?
they are non-opioid analgesics
they mainly act on nociceptive pain
What is the mode of action of NSAIDs?
they inhibit the enzyme cyclooxygenase (COX)
this consequently inhibits prostaglandin synthesis
by inhibiting prostaglandins, this reduces tissue inflammation and pain

What are the stages involved in prostaglandin synthesis?
- cell membrane phospholipids are converted to arachidonic acid by phospholipase A2
- arachidonic acid is converted to PGG and PGH by cyclooxygenase
- PGG and PGH go on to form prostaglandins and thromboxane

Why are NSAIDs said to be ‘non-selective’?
they will inhibit both COX-1 and COX-2 enzymes in a ratio that varies from drug to drug
selective COX-2 inhibitors are more potent at inhibiting COX-2 enzyme