Histology-Female Reproductive System Flashcards
(81 cards)
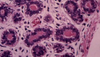
What structures are indicated in the image below?

What structures are indicated in the image below? T= tunica albuguinea connective tissue. F = follicles in cortex. M = medulla with lots of blood vessels and cells that make estrogen and progesterone.
What cells are the origin of the majority of ovarian cancers?
Surface epithelial cells account for 70% of all ovarian tumors and 90% of malignant ovarian tumors.

What cells are indicated below?

Surface epithelial (germinal epithelium) layers of the ovary. Note the simple cuboidal epithelium lying on top of the tunica albuginea connective tissue. Finally, you know you are in the ovary because you see follicles at all stages of development embedded in a stroma (note the dying follicle indicated by the black arrow).
How do follicles form during embryogenesis?
Primordial germ cells migrate from the yolk sac to the genital ridge in the embryo. The mesodermal cells from the genital ridge divide and surround the germ cells. This forms follicles.
Oocyte stem cells, what are they doing around 4 months gestation?
Oogonia. They divide by mitosis and form germ cell clusters, bridges and sync up to the same stage of mitosis.

What is happening to the female germ cells around the 7th month of gestation?
Oogonia stem cells have entered meiosis and become an oocyte. At this point they are surrounded by follicular cells.

What is happening to the female germ cells around birth?
Nothing, they are in dictyotene stage (arrested in metaphase I of meiosis I). If the oocyte is not in a primordial follicle at birth, it dies. Early in life the pool of oocytes in the ovary is fixed.

What makes up a follicle?
Oocyte + surrounding follicular cells.
When do the majority of oocytes die? Why do we lose so many between birth and puberty?
In utero. Also note that you decrease from 700,000 follicles at birth to 400,000 at puberty because primordial follicles are continually recruited for growth, but die due to lack of FSH secretion.

What is responsible for the different maturity levels of follicles shown in the ovarian cortex below?

Kisspeptin release from the hypothalamus stimulates GnRH secretion to initiate puberty. FSH is released and stimulates follicles to mature into a Graafian follicle. One follicle will have lots of FSH receptors, grow to a large size, secrete lots of estrogen and feedback inhibit FSH release from the pituitary. This causes atresia of the other follicles.

What follicles are you responsible for knowing?
Primordial follicle -> Growing follicle -> Vesicular follicle -> Mature (Graffian follicle)

What type of follicle is this?

Note the oocyte in the center and simple squamous covering. This is a primordial follicle and is quiescent until it gets hormonal signaling to divide.

What type of follicle is this?

Note the taller epithelial cells and increasing layers of granulosa cells (follicular epithelium). This indicates a growing follicle.

How do oocytes communicate with the follicle cells surrounding it?
There are gap junctions

What do glycoproteins form around the oocyte in the growing ovarian follicle? What cells transport oxygen and nutrients from the basement membrane of the oocyte and through the zona pellucida?
Zona pellucida = glycoprotein layer that induces acrosome reaction. Granulosa layer: rests on BM and transports nutrients to oocyte through zona pellucida, note that these also secrete estrogen.

How does the oocyte of a growing follicle differ from that of a primordial follicle?
The growing follicle is larger, has a thicker zona pellucida and the granulosa layer (follicular layer) is more organized.

What structures pierce the zona pellucida?
Oocyte cytoplasm and follicular cell cytoplasm. They communicate via gap junctions.

Other names for a vesicular follicle?
Secondary or antral follicle
What type of follicle is shown below?

Note that the fluid secreted by the granulosa cells forms and empty space (antrum). Also note the theca interna and theca externa. This is a vesicular ovarian follicle.

What substance secreted by the granulosa cells is key in maintaining the quiescent status of an oocyte?
Oocyte maturation inhibitor, it is contained within the antrum.
What substance is secreted by the theca interna?
Androgen. It is converted to estrogen by the aromatase of the granulosa cells.
What type of follicle is indicated in the image below?

Note that all of the antra have coalesced to from one giant antrum. Note that mural granulosa cells are covering the wall of the follicle and cumulus oophorus granulosa cells are covering the wall of the oocyte, forming the corona radiata. This is a mature/Graafian follicle.

What interchange is going on between the cumulus oophorus and the mural granulosa cells?
Mural granulosa cells are producing the oocyte maturation inhibitor and the cumuli oophorus have the receptors for the inhibiting factor.
What structures are indicated in the image below from an ovarian ultrasound?

This is a Graafian follicle: 1) Ovarian tissue 2) Follicle about to rupture 3) Remains of pedicle 4) Follicular diameter > 10mm.