Pathoma Ch 1-2 Flashcards
(56 cards)
Hyperplasia vs Hypertrophy with mechanisms
3 tissues that can only undergo hypertrophy
Hyperplasia: increase in cell number from STEM cells
Hypertrophy: increase in cell size from gene activation a, protein synthesis, and production of organelles.
- cardiac cells
- skeletal muscle cells
- nerves
Two ways that atrophy can occur
- Decrease in cell number via apoptosis
- Decrease in cell size via:
a. Ubiquitin-proteosome degredation (intermediate filaments are tagged and destroyed by proteosomes)
b. autophagy (vacuoles fuse with lysosomes whose hydrolytic enzymes breakdown cellular components)
Metaplasia (what is it, mechanism, example)
- change in stress leading to change in cell type
- occurs via reprogramming of stem cells, which then produce the new cell type
- is REVERSIBLE
Metaplasia –> Dysplasia –> Cancer if persistent stress
ex: Barrett esophagus, Vitamin A deficiency (columnar cells of conjunctiva –> keratinizing squamous cells), Myositis Ossificans

Dysplasia
Aplasia
Hypoplasia
Dysplasia: disordered cell growth. Proliferation of precancerous cells. Ex: cervical intraepithelial neoplasia (CIN). Arise from longstanding hyperplasia or metaplasia
Aplasia: failure of cell production during embryogenesis (unilateral renal agensis)
Hypoplasia: decrease in cell production during embryogenesis (steak ovary in Turner Syndrome)
Ischemia and 3 types of it
decreased blood flow through an organ
- Decrease arterial profusion (atherosclerosis)
- Decrease venous drainage (budd chiari syndrome –> caused by polycythemia vera, which is increased RBC due to overproduction)
- Shock: generalized hypotension resulting in poor tissue perfusion
Hypoxemia, what is it and what are 4 examples
low partial pressure of oxygen in the blood (PaO2<60)
- High altitude (decreased PAO2)
- Hypoventilation (increased PACO2 –> decreased PA02)
- Diffusion defect (thicker diffusion barrier like in interstitial pulmonary fibrosis)
- V/Q mismatch: blood bypass oxygenated lung (right to left shunt) or oxygenated air cannot reach blood (atelectasis)
Methemoglobinemia
Fe2+ carries oxygen.
Fe2+ –> Fe3+ in methemoglobinemia, cannot bind oxygen. PaO2 normal, SaO2 decreased
-seen with odidant stress (sulfa and nitrate drugs)
Presentation: cyanosis with chocolate colored blood
Tx: Methylene blue (converts Fe3+ –> Fe2+)

3 problems associated with low ATP
- Na/K pump cannot run, resulting in increased Na in cell leading to increased H20 in cell.
- Ca pump not work, resulting in increased Ca in cytosol
- Aerobic glycolysis –> anaerobic glycolysis –> production of lactic acid
Early vs late stage cellular injury from hypoxia
Early: hallmark is Cellular Swelling (reverisble)
results in loss of microvilli and blebbing, swelling of RER leading to loss of protein synthesis
Late: hallmark is membrane damage (irreversible)
- plasma membrane damage (troponin leak out)
- Mitochondrial membrane damage (cytochrome C leak out)
- Lysosome membrane damage (hydrolytic enzymes leak out, activated by Ca2+)
6 types of necrosis with mechanisms and examples of each
- Coagulative Necrosis: remains FIRM. ischemic infarction of any organ EXCEPT BRAIN. wedged shaped. Seen 1-3 days post MI
- Liquefactive Nectrosis: Brain (via microglial cells), Abscess (enzymes of neutrophils), Pancreatitis (enzymes of pancreas autodigest)
- Gangrenous necrosis: coagulative necrosis that resembles mummified tissue. ischemia of lower limb and GI
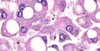
- Caseous necrosis: soft and friable, combo of liquefactive and coagulative. Seen in TB/Fungal where granulomas form
- Fat necrosis: chalky white due to Ca deposition. Trauma of fat –> saponification
- Fibrinoid Necrosis: damage to blood vessel wall. Bright pink staining (fibrin). Malignant hypertension and vasculitis
Activation of capsases (which are responsible for mediating apoptosis via activation of proteases and endonucleases)
3 ways
- Intrinsic mitochondrial pathway: inactivation of Bcl2 allows cytochrome C to leak from mito matrix
- Extrinsic receptor ligand: FAS binds FAS death receptor (CD95) to activate capsase
- Cytotoxic CD8+: Perforins create pores, Granzymes enter pores and activate capsaes
3 types of free radicals and how do they cause cellular injury (2)
- O2- (superoxide)
- H2O2 (hydrogen peroxide)
- OH (hydroxyl radical) **the most damaging**
cause injury via
- peroxidation of lipids
- oxidation of DNA and proteins
Elimination of free radicals via 3 mechanisms in body
- antioxidants (glutathione, Vitamin A,C,E)
- Enzymes:
- superoxide dismutase for O2 –> H2O2
- glutathione peroxidase for OH
- catalase (in peroxisomes) for H2O2 - Metal carrier proteins (transferrin and ceruplasmin)
Carbon tetrachloride (CCl4)
solvent used in dry cleaning industry
-converted to CCl3, results in cell injury with swelling of RER and results in decreased apolipoprotein –> fatty change in liver
Mediators that attract nutrophils
- leukotriene b4 (LTB4 is a neutrophil chemotactic agent. Neutrophils arrive B4 others)
- IL-8
- C5A
- Bacterial products
2 reasons that you get acute inflammation
(neutrophils + edema)
- In response to infection (to eliminate pathogen)
- Tissue necrosis (to clear necrotic debris)
5 mediators of acute inflammation (overview)
- Toll-like receptors
- Arachidonic Acid metabolites
- Mast Cells
- Complement
- Hageman Factor (Factor XII)
Toll-like receptors (TLR)
Present on macrophages and dendritic cells (innate)
CD14 (co-receptor for TLR-4) on macrophages recognizes lipopolysaccharide (PAMP) on outter membrane Gram - bacteria
-Results in upregulation of NFKB

Arachadoinic Acid pathway overview
AA is released from the phospholipid cell membane by phospholipase A2 amd then acted upon by cyclooxygenase or 5-lipoxygenase
cyclooxygenase –> prostaglandins (mediate vasodilation, increased vascular permability) PGE2 mediate pain and fever
5-lipoxygenase –> leukotriene (mediate vasoconstriction, bronchospasm, increased vascular permeability via pericytes)

Mast Cells activated by 3 things
- Tissue trauma
- Complement C3a and C5a
- Cross-linking of cell-surface IgE by antigen
- release pre-formed histamine granules, which mediate vasodilation of arterioles and increase vascular permeability
Complement System 3 pathways of activation
System of hepatically synthesized plasma proteins that play a role in innate immunity and inflammation. Membrane attack complex (MAC) defends against gram-negative bacteria.
1. Classical: C1 binds IgG and IgM (GM makes classic cars)
2. Alternative: microbial products directly activate
3. Mannose-binding lectin (MBL): MBL binds mannose on miccroorganisms
Complement pathway (general overview)
All pathways result in production of C3 convertase, which in turn produces C5 convertase.
C5b complexes with C6-C9 to form the MAC
C3b—opsonization.
C3a, C4a, C5a—anaphylaxis.
C5a—neutrophil chemotaxis.

Hageman factor (Factor XII)
Inactive pro-inflammatory protein produced in liver
Activated in response to exposure to subendothelial or tissue collagen
Activates clotting cascade when exposed to subendothlial collagen












