Autoimmune Diseases 2 Flashcards
(81 cards)
Non-genetic factors in autoimmunity: Infection
- Some infections have been linked with the subsequent development of autoimmune disease
- An immunological explanation is known as … …, in which epitopes relevant to the pathogen are shared with host antigens
- Some infections have been linked with the subsequent development of autoimmune disease
- An immunological explanation is known as molecular mimicry, in which epitopes relevant to the pathogen are shared with host antigens
Molecular mimicry
- Viral infection: presentation of viral peptides to a CD4 T cell via MHC …, causing T cell activation
- The viral peptides happen to be similar to a host-derived peptide; the T cell would normally recognise these peptides, but would not react to them
- The activated T cell now reacts strongly to the self-peptide and initiates …
- The process depends on having the correct MHC molecules to present this critical epitope that is common to both virus and host (inherited)
- Also depends on having the correct T cell to recognise it (mainly bad luck)
- Viral infection: presentation of viral peptides to a CD4 T cell via MHC 2, causing T cell activation
- The viral peptides happen to be similar to a host-derived peptide; the T cell would normally recognise these peptides, but would not react to them
- The activated T cell now reacts strongly to the self-peptide and initiates inflammation
- The process depends on having the correct MHC molecules to present this critical epitope that is common to both virus and host (inherited)
- Also depends on having the correct T cell to recognise it (mainly bad luck)

Molecular mimicry
- Viral infection: presentation of viral peptides to a CD4 T cell via MHC 2, causing T cell activation
- The viral peptides happen to be similar to a host-derived peptide; the T cell would normally recognise these peptides, but would not react to them
- The activated T cell now reacts strongly to the self-peptide and initiates inflammation
- The process depends on having the correct MHC molecules to present this critical epitope that is common to both virus and host (…)
- Also depends on having the … to recognise it (mainly bad luck)
- Viral infection: presentation of viral peptides to a CD4 T cell via MHC 2, causing T cell activation
- The viral peptides happen to be similar to a host-derived peptide; the T cell would normally recognise these peptides, but would not react to them
- The activated T cell now reacts strongly to the self-peptide and initiates inflammation
- The process depends on having the correct MHC molecules to present this critical epitope that is common to both virus and host (inherited)
- Also depends on having the correct T cell to recognise it (mainly bad luck)

Molecular mimicry
- Viral …: presentation of viral peptides to a CD4 T cell via MHC 2, causing T cell activation
- The viral peptides happen to be similar to a host-derived peptide; the T cell would normally recognise these peptides, but would not react to them
- The activated T cell now reacts strongly to the self-peptide and initiates inflammation
- The process depends on having the correct MHC molecules to present this critical epitope that is common to both virus and host (inherited)
- Also depends on having the correct T cell to recognise it (mainly bad luck)
- Viral infection: presentation of viral peptides to a CD4 T cell via MHC 2, causing T cell activation
- The viral peptides happen to be similar to a host-derived peptide; the T cell would normally recognise these peptides, but would not react to them
- The activated T cell now reacts strongly to the self-peptide and initiates inflammation
- The process depends on having the correct MHC molecules to present this critical epitope that is common to both virus and host (inherited)
- Also depends on having the correct T cell to recognise it (mainly bad luck)

Molecular mimicry
- Viral infection: presentation of viral peptides to a CD4 T cell via MHC 2, causing T cell activation
- The viral peptides happen to be similar to a host-derived peptide; the T cell would normally recognise these peptides, but would not react to them
- The activated T cell now … strongly to the self-peptide and initiates …
- The process depends on having the correct MHC molecules to present this critical epitope that is common to both virus and host (inherited)
- Also depends on having the correct T cell to recognise it (mainly bad luck)
- Viral infection: presentation of viral peptides to a CD4 T cell via MHC 2, causing T cell activation
- The viral peptides happen to be similar to a host-derived peptide; the T cell would normally recognise these peptides, but would not react to them
- The activated T cell now reacts strongly to the self-peptide and initiates inflammation
- The process depends on having the correct MHC molecules to present this critical epitope that is common to both virus and host (inherited)
- Also depends on having the correct T cell to recognise it (mainly bad luck)

Give 2 examples of molecular mimicry
-
Autoimmune haemolysis after Mycoplasma pneumoniae
- Mycoplasma antigen has homology to ‘I’ antigen on red blood cells
- IgM antibody to mycoplasma may cause transient haemolysis
-
Rheumatic fever: inflammatory disease occurring after streptococcal infection affecting heart, joints, skin and brain
- Anti-streptococcal antibodies believed to cross-react with connective tissue
- Even for these ‘best examples’ the target antigens are not well-defined; for other diseases the paradigm remains rather theoretical
Autoimmune haemolysis after Mycoplasma pneumoniae is an example of molecular …
-
molecular mimicry
- Autoimmune haemolysis after Mycoplasma pneumoniae
- Mycoplasma antigen has homology to ‘I’ antigen on red blood cells
- IgM antibody to mycoplasma may cause transient haemolysis
Rheumatic fever is an example of molecular …
-
molecular mimicry
- It is an inflammatory disease occurring after streptococcal infection affecting heart, joints, skin and brain
- Anti-streptococcal antibodies believed to cross-react with connective tissue
Autoimmune haemolysis after Mycoplasma pneumoniae
- Mycoplasma antigen has homology to ‘I’ antigen on red blood cells
- Ig… antibody to mycoplasma may cause transient …
- Mycoplasma antigen has homology to ‘I’ antigen on red blood cells
- IgM antibody to mycoplasma may cause transient haemolysis
Rheumatic fever
- It is an inflammatory disease occurring after … infection affecting heart, joints, skin and brain
- Anti-… antibodies believed to cross-react with connective tissue
- It is an inflammatory disease occurring after streptococcal infection affecting heart, joints, skin and brain
- Anti-streptococcal antibodies believed to cross-react with connective tissue
Type 1 diabetes
- Lack of insulin impairs cellular update of glucose, leading to polyuria, polydypsia, polyphagia and weight loss
- Onset at any age, but typically …
- Disease prevalence around …%; rising by around 5% per anum
- Treatment by injection of insulin and diet
- Important to differentiate from:
- … diabetes - can present with a similar phenotype but requires different management
- Type II diabetes mellitus = older onset, insulin secretion, ketoacidosis less likely and insulin not necessarily required
- Lack of insulin impairs cellular update of glucose, leading to polyuria, polydypsia, polyphagia and weight loss
- Onset at any age, but typically childhood
- Disease prevalence around 0.8%; rising by around 5% per anum
- Treatment by injection of insulin and diet
- Important to differentiate from:
- Monogenic diabetes - can present with a similar phenotype but requires different management
- Type II diabetes mellitus = older onset, insulin secretion, ketoacidosis less likely and insulin not necessarily required
Type 1 diabetes
- Lack of insulin impairs cellular update of glucose, leading to polyuria, polydypsia, polyphagia and weight …
- Onset at any age, but typically childhood
- Disease prevalence around 0.8%; rising by around …% per anum
- Treatment by injection of insulin and diet
- Important to differentiate from:
- Monogenic diabetes - can present with a similar phenotype but requires different management
- Type II diabetes mellitus = older onset, insulin secretion, ketoacidosis less likely and insulin not necessarily required
- Lack of insulin impairs cellular update of glucose, leading to polyuria, polydypsia, polyphagia and weight loss
- Onset at any age, but typically childhood
- Disease prevalence around 0.8%; rising by around 5% per anum
- Treatment by injection of insulin and diet
- Important to differentiate from:
- Monogenic diabetes - can present with a similar phenotype but requires different management
- Type II diabetes mellitus = older onset, insulin secretion, ketoacidosis less likely and insulin not necessarily required
Immunology of type 1 diabetes
- Evidence for … disease
- Islet cell antibodies detectable for months to years before the onset of clinical disease
- HLA associations
- Mouse model
- Early pancreatic biopsy shows … with CD4/ 8 T cells
- Note that although antibodies present, they do not appear to be directly relevant to destruction of the pancreas
- By the time patient has established diabetes, generally no active inflammation in pancreatic biopsy
- Evidence for autoimmune disease
- Islet cell antibodies detectable for months to years before the onset of clinical disease
- HLA associations
- Mouse model
- Early pancreatic biopsy shows infiltration with CD4/ 8 T cells
- Note that although antibodies present, they do not appear to be directly relevant to destruction of the pancreas
- By the time patient has established diabetes, generally no active inflammation in pancreatic biopsy

Immunology of type 1 diabetes
- Is there evidence for autoimmune disease?
- Yes - Evidence for autoimmune disease
- Islet cell antibodies detectable for months to years before the onset of clinical disease
- HLA associations
- Mouse model
- Early pancreatic biopsy shows infiltration with CD4/ 8 T cells
- Note that although antibodies present, they do not appear to be directly relevant to destruction of the pancreas
- By the time patient has established diabetes, generally no active inflammation in pancreatic biopsy

This is a pancreatic biopsy showing what?

pre-diabetic pancreatic biopsy showing infiltration with CD8 T cells
Progression to type 1 diabetes
- Fill in the blanks


Progression to Type 1 diabetes
- By the time overt diabetes has developed, over …% of the pancreas has been destroyed
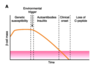
- By the time overt diabetes has developed, over 90% of the pancreas has been destroyed
Genetics and type 1 diabetes
- Genetic background definitely important – conconcordance in monozygotic twins is close to 100% if they are observed for long enough (nb older texts underestimate this risk)
- … class II alleles are the major defined genetic risk factor
- DR3 or DR4 relative risk is 6
- DR3 and DR4 relative risk is 15
- Rather like coeliac disease, believed that these molecules are required to present relevant islet cell antigens to CD4 T cells
- Autoimmune response may occur if appropriate T cell receptors are present, together with other … and … co-factors
- Genetic background definitely important – conconcordance in monozygotic twins is close to 100% if they are observed for long enough (nb older texts underestimate this risk)
-
HLA class II alleles are the major defined genetic risk factor
- DR3 or DR4 relative risk is 6
- DR3 and DR4 relative risk is 15
- Rather like coeliac disease, believed that these molecules are required to present relevant islet cell antigens to CD4 T cells
- Autoimmune response may occur if appropriate T cell receptors are present, together with other genetic and environmental co-factors
Genetics and type 1 diabetes
- Is Genetic background definitely important?
- yes - Genetic background definitely important – conconcordance in monozygotic twins is close to 100% if they are observed for long enough (nb older texts underestimate this risk)
- HLA class II alleles are the major defined genetic risk factor
- DR3 or DR4 relative risk is 6
- DR3 and DR4 relative risk is 15
- Rather like coeliac disease, believed that these molecules are required to present relevant islet cell antigens to CD4 T cells
- Autoimmune response may occur if appropriate T cell receptors are present, together with other genetic and environmental co-factors
… class II alleles are the major defined genetic risk factor for T1 diabetes
-
HLA class II alleles are the major defined genetic risk factor
- –DR3 or DR4 relative risk is 6
- –DR3 and DR4 relative risk is 15
What is the major defined genetic risk factor for T1 diabetes?
HLA class II alleles are the major defined genetic risk factor for T1 diabetes
Precipitating events - T1 diabetes
- … to islet cell antigens present for months-years before onset of clinical disease
- Gap between initiation of disease and its presentation makes identification of triggers difficult
- Much of the data is epidemiological
- Some evidence for … virus
- Stronger immune response to virus in cases compared to controls
- Viral infection can cause pancreatitis in mice and humans, and precipitate autoimmune diabetes in mouse models
- Protein 2C from Coxsackie virus has homology with islet cell antigen glutamic acid decarboxylase (GAD) (?molecular mimicry mechanism)
- Autoantibodies to islet cell antigens present for months-years before onset of clinical disease
- Gap between initiation of disease and its presentation makes identification of triggers difficult
- Much of the data is epidemiological
- Some evidence for Coxsackie virus
- Stronger immune response to virus in cases compared to controls
- Viral infection can cause pancreatitis in mice and humans, and precipitate autoimmune diabetes in mouse models
- Protein 2C from Coxsackie virus has homology with islet cell antigen glutamic acid decarboxylase (GAD) (?molecular mimicry mechanism)
Precipitating events - T1 diabetes
- Autoantibodies to islet cell antigens present for months-years before onset of clinical disease
- Gap between … of disease and its … makes identification of triggers difficult
- Much of the data is epidemiological
- Some evidence for Coxsackie virus
- Stronger immune response to virus in cases compared to controls
- Viral infection can cause pancreatitis in mice and humans, and precipitate autoimmune diabetes in mouse models
- Protein 2C from Coxsackie virus has homology with islet cell antigen glutamic acid decarboxylase (GAD) (?molecular mimicry mechanism)
- Autoantibodies to islet cell antigens present for months-years before onset of clinical disease
- Gap between initiation of disease and its presentation makes identification of triggers difficult
- Much of the data is epidemiological
- Some evidence for Coxsackie virus
- Stronger immune response to virus in cases compared to controls
- Viral infection can cause pancreatitis in mice and humans, and precipitate autoimmune diabetes in mouse models
- Protein 2C from Coxsackie virus has homology with islet cell antigen glutamic acid decarboxylase (GAD) (?molecular mimicry mechanism)
Summary: The development of AID is multi-step
- … background: Critical for some diseases in determining which peptides can be presented
- T cell receptor …: critical in determining whether the peptide-MHC complex can be recognised. Note: the gene segments are inherited, but the receptors are produced randomly and will differ even in identical twins
- Infection: may influence the activation of T cells and B cells that are potentially auto reactive
- Likely to be myriad other genetic and environmental factors
- MHC background: Critical for some diseases in determining which peptides can be presented
- T cell receptor repertoire: critical in determining whether the peptide-MHC complex can be recognised. Note: the gene segments are inherited, but the receptors are produced randomly and will differ even in identical twins
- Infection: may influence the activation of T cells and B cells that are potentially auto reactive
- Likely to be myriad other genetic and environmental factors































