Mucosal Immunology 1 Flashcards
(53 cards)
MALT, BALT, GALT
- The mucosa-associated lymphatic tissue (MALT) is divided into
- BALT (…-associated lymphatic tissue)
- and
- GALT (… -associated lymphatic tissue)
- The mucosa-associated lymphatic tissue (MALT) is divided into
- BALT (bronchus-associated lymphatic tissue)
- and
- GALT (gut -associated lymphatic tissue)
MALT, BALT, GALT
- The …-associated lymphatic tissue (MALT) is divided into
- BALT (bronchus-associated lymphatic tissue)
- and
- GALT (gut -associated lymphatic tissue)
- The mucosa-associated lymphatic tissue (MALT) is divided into
- BALT (bronchus-associated lymphatic tissue)
- and
- GALT (gut -associated lymphatic tissue)
Why is the mucosal immune system so very important?
- It is the … immune compartment of the organism
- With an estimated surface area of 400 m2 it harbours …% of all effector cells
- It is in direct contact with the outside environment
- There is continuous antigen stimulation (food, endogenous flora, & pathogens)
- Mucosal sites are the ports of entry for many infections and an important target site for vaccine-induced protection
- It is the biggest immune compartment of the organism
- With an estimated surface area of 400 m2 it harbours 60% of all effector cells
- It is in direct contact with the outside environment
- There is continuous antigen stimulation (food, endogenous flora, & pathogens)
- Mucosal sites are the ports of entry for many infections and an important target site for vaccine-induced protection
Why is the mucosal immune system so very important?
- It is the biggest immune compartment of the organism
- With an estimated surface area of 400 m2 it harbours 60% of all effector cells
- It is in direct contact with the … environment
- There is … antigen stimulation (food, endogenous flora, & pathogens)
- Mucosal sites are the ports of entry for many infections and an important target site for vaccine-induced protection
- It is the biggest immune compartment of the organism
- With an estimated surface area of 400 m2 it harbours 60% of all effector cells
- It is in direct contact with the outside environment
- There is continuous antigen stimulation (food, endogenous flora, & pathogens)
- Mucosal sites are the ports of entry for many infections and an important target site for vaccine-induced protection
Why is the mucosal immune system so very important?
- It is the biggest immune compartment of the organism
- With an estimated surface area of 400 m2 it harbours 60% of all effector cells
- It is in … contact with the outside environment
- There is continuous … stimulation (food, endogenous flora, & pathogens)
- Mucosal sites are the ports of entry for many infections and an important target site for vaccine-induced protection
- It is the biggest immune compartment of the organism
- With an estimated surface area of 400 m2 it harbours 60% of all effector cells
- It is in direct contact with the outside environment
- There is continuous antigen stimulation (food, endogenous flora, & pathogens)
- Mucosal sites are the ports of entry for many infections and an important target site for vaccine-induced protection
Why is the mucosal immune system so very important?
- It is the biggest immune compartment of the organism
- With an estimated surface area of 400 m2 it harbours 60% of all effector cells
- It is in direct contact with the outside environment
- There is continuous antigen stimulation (food, endogenous flora, & pathogens)
- Mucosal sites are the ports of entry for many … and an important target site for …-induced protection
- It is the biggest immune compartment of the organism
- With an estimated surface area of 400 m2 it harbours 60% of all effector cells
- It is in direct contact with the outside environment
- There is continuous antigen stimulation (food, endogenous flora, & pathogens)
- Mucosal sites are the ports of entry for many infections and an important target site for vaccine-induced protection
… sites are the ports of entry for many infections and an important target site for vaccine-induced protection
Mucosal sites are the ports of entry for many infections and an important target site for vaccine-induced protection
Mucosal surfaces are a prime site of entry for … pathogens
Mucosal surfaces are a prime site of entry for infectious pathogens
… surfaces are a prime site of entry for infectious pathogens
Mucosal surfaces are a prime site of entry for infectious pathogens

- Most of the pathogens that cause the deaths of large numbers of people are those of mucosal surfaces or enter the body through these routes. The genitourinary, rectal and oral mucosa are the main mucosal transmission routes for … infection, for example.
- If a vaccine could induce both … and local mucosal immunity it would offer the best possible protection against mucosal … transmission and ….
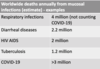
- Most of the pathogens that cause the deaths of large numbers of people are those of mucosal surfaces or enter the body through these routes. The genitourinary, rectal and oral mucosa are the main mucosal transmission routes for HIV infection, for example.
- If a vaccine could induce both systemic and local mucosal immunity it would offer the best possible protection against mucosal HIV transmission and AIDS.
1. The main defence strategies of intestinal mucosa & oropharynx (1)
- Endogenous …
- 1014 bacteria, hundreds of different species (10x more than all cells in the human body)
- Epithelium and …
- Mechanical … (cells, tight junctions)
- Mucins (extensively glycosylated proteins) form a viscous barrier
- … epithelial cells (goblet cells, absorptive epithelial cells, M cells, Paneth cells)
- … substances (defensins, lysozyme, lactoferrin, phospholipases )
- Endogenous flora
- 1014 bacteria, hundreds of different species (10x more than all cells in the human body)
- Epithelium and Mucus
- Mechanical Barriers (cells, tight junctions)
- Mucins (extensively glycosylated proteins) form a viscous barrier
- Specialised epithelial cells (goblet cells, absorptive epithelial cells, M cells, Paneth cells)
- Antimicrobial substances (defensins, lysozyme, lactoferrin, phospholipases )
1. The main defence strategies of intestinal mucosa & oropharynx (1)
- … flora
- 1014 bacteria, hundreds of different species (10x more than all cells in the human body)
- Epithelium and Mucus
- … Barriers (cells, tight junctions)
- Mucins (extensively … proteins) form a viscous barrier
- Specialised epithelial cells (goblet cells, absorptive epithelial cells, M cells, Paneth cells)
- … substances (defensins, lysozyme, lactoferrin, phospholipases )
-
Endogenous flora
- 1014 bacteria, hundreds of different species (10x more than all cells in the human body)
- Epithelium and Mucus
- Mechanical Barriers (cells, tight junctions)
- Mucins (extensively glycosylated proteins) form a viscous barrier
- Specialised epithelial cells (goblet cells, absorptive epithelial cells, M cells, Paneth cells)
- Antimicrobial substances (defensins, lysozyme, lactoferrin, phospholipases )
1. The main defence strategies of intestinal mucosa & oropharynx (2)
- (3) Regionalised Immune System
- Waldeyer’s ring (lingual and palatine tonsils, nasopharyngeal tonsils)
- …´s patches
- In Part II:
- … lymph nodes
- Intraepithelial immune cells
- Lamina … immune cells
- (4) Gut homing of B and T cells
- Immune cells primed in the induction sites return to the relevant effector sites (homing)
- (3) Regionalised Immune System
- Waldeyer’s ring (lingual and palatine tonsils, nasopharyngeal tonsils)
- Peyer´s patches
- In Part II:
- Mesenteric lymph nodes
- Intraepithelial immune cells
- Lamina propria immune cells
- (4) Gut homing of B and T cells
- Immune cells primed in the induction sites return to the relevant effector sites (homing)

1. The main defence strategies of intestinal mucosa & oropharynx (2)
- (3) Regionalised Immune System
- Waldeyer’s ring (lingual and palatine tonsils, nasopharyngeal tonsils)
- …´s patches
- In Part II:
- Mesenteric lymph nodes
- Intraepithelial immune cells
- Lamina propria immune cells
- (4) Gut … of B and T cells
- Immune cells primed in the induction sites return to the relevant effector sites (homing)
- (3) Regionalised Immune System
- Waldeyer’s ring (lingual and palatine tonsils, nasopharyngeal tonsils)
- Peyer´s patches
- In Part II:
- Mesenteric lymph nodes
- Intraepithelial immune cells
- Lamina propria immune cells
- (4) Gut homing of B and T cells
- Immune cells primed in the induction sites return to the relevant effector sites (homing)

… is a major factor in maintaining a healthy composition of the micro-organisms living in the gut. Microbiota and microbiome are often used interchangeably, however, ‘microbiota’ technically speaking refers to the actual microorganisms whereas the ‘microbiome’ refers to the totality of their genes
Diet is a major factor in maintaining a healthy composition of the micro-organisms living in the gut. Microbiota and microbiome are often used interchangeably, however, ‘microbiota’ technically speaking refers to the actual microorganisms whereas the ‘microbiome’ refers to the totality of their genes
… is a major factor in maintaining a healthy composition of the micro-organisms living in the gut.
Diet is a major factor in maintaining a healthy composition of the micro-organisms living in the gut.

1. The main defence strategies of intestinal mucosa & oropharynx (8)
- (1) … diet
- Rich in fibre, supports healthy gut microbiota
- … produced by bacteria
- Increased mucus production, increased antimicrobial peptide production
- Increased expression of tight junction proteins
- (2) Typical ‘…’ diet
- Low in fibre
- Diversity of bacteria …
- … SCFA production
- More (chronic) inflammation
- leakiness
- (1) Prudent diet
- Rich in fibre, supports healthy gut microbiota
- SCFAs produced by bacteria
- Increased mucus production, increased antimicrobial peptide production
- Increased expression of tight junction proteins
- (2) Typical ‘Western’ diet
- Low in fibre
- Diversity of bacteria reduced
- Low SCFA production
- More (chronic) inflammation
- leakiness

1. The main defence strategies of intestinal mucosa & oropharynx (8)
- (1) Prudent diet
- Rich in …, supports healthy gut microbiota
- SCFAs produced by bacteria
- … mucus production, … antimicrobial peptide production
- … expression of tight junction proteins
- (2) Typical ‘Western’ diet
- Low in …
- Diversity of bacteria reduced
- Low SCFA production
- More (chronic) inflammation
- l…
- (1) Prudent diet
- Rich in fibre, supports healthy gut microbiota
- SCFAs produced by bacteria
- Increased mucus production, increased antimicrobial peptide production
- Increased expression of tight junction proteins
- (2) Typical ‘Western’ diet
- Low in fibre
- Diversity of bacteria reduced
- Low SCFA production
- More (chronic) inflammation
- leakiness

Prudent diet
- Rich in …, supports healthy gut …
- SCFAs (short chain FA) produced by bacteria
- Increased … production, increased antimicrobial peptide production
- Increased expression of tight … proteins
- Rich in fibre, supports healthy gut microbiota
- SCFAs (short chain FA) produced by bacteria
- Increased mucus production, increased antimicrobial peptide production
- Increased expression of tight junction proteins
Typical ‘Western’ diet
- Low in …
- … of bacteria reduced
- … SCFA production
- More (…) inflammation
- leakiness
- Low in fibre
- Diversity of bacteria reduced
- Low SCFA production
- More (chronic) inflammation
- leakiness
Intestinal Epithelial Cells (1)
- Epithelial cells:
- …
- TLRs (TLR2,4,5,6,7,9 depending on region of gut).
- TLR5 on … surface activated by bacteria.
- NLR in cytoplasm activated by … (invading bacteria)
- Epithelial cells:
- Microvilli
- TLRs (TLR2,4,5,6,7,9 depending on region of gut).
- TLR5 on basolateral surface activated by bacteria.
- NLR in cytoplasm activated by flagellins (invading bacteria)

… at basolateral surface tightens tight junctions upon contact with bacteria
TLR5 at basolateral surface tightens tight junctions upon contact with bacteria

TLR5 at … surface tightens tight junctions upon contact with bacteria
TLR5 at basolateral surface tightens tight junctions upon contact with bacteria

Intestinal Epithelial Cells (2) (Paneth, Goblet and M Cells)
- Paneth cells
- produce human … 5 (HD5) precursor & HD6 precursor,
- … (activates HD5 and HD6 by proteolytic cleavage
- Goblet cells
- Produce … as a physicochemical barrier
- Antibacterial peptides and antibodies of IgG secretory IgA type are dispersed in the mucus
- (-> transepithelial transport of IgA)
- M cells
- transport … from gut lumen to subepithelial lymphoid structures (-> Peyer’s patches)
- Paneth cells
- produce human defensin 5 (HD5) precursor & HD6 precursor,
- Trypsin (activates HD5 and HD6 by proteolytic cleavage
- Goblet cells
- Produce mucus as a physicochemical barrier
- Antibacterial peptides and antibodies of IgG secretory IgA type are dispersed in the mucus
- (-> transepithelial transport of IgA)
- M cells
- transport antigens from gut lumen to subepithelial lymphoid structures (-> Peyer’s patches)






































