Cranial Trauma Flashcards
(150 cards)
A 78-year-old man was admitted to hospital with a 2 week history of progressive confusion and unsteadiness. His medical history included parkinsonism and a metallic mitral valve replacement. On examination his GCS was 14/15 (E4, V4, M6) and he had left-sided weakness. He was
taking warfarin, and the INR was 3.8.
DDx?
Progressive confusion and gait disturbance with left hemiparesis point to right hemisphere lesion.
DDx includes:
Cerebral infarction/haemorrhage
Subdural haematoma
Neoplastic lesion
Progressive symptoms suggest a slowly enlarging mass such as a tumour or chronic subdural haematoma
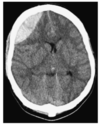
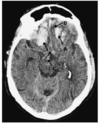
Describe the CT

Extra-axial cresent shaped fluid collection over the right cerebral convexity (A,B) indiacting chronic SDH
As patient is supine, there is layering according to density, wthi hypodense fluid supernatant (A) above hyperdense thrombus or cellular precipitant.
This could be due to a single episode of heamorrhage or rebleeding into a chronic collection.
There is midline shift (C) with obliteration of cerebral sulci and the trigone not seen on the right
Pathophysiology of chronic SDHs
Typically caused by tearing of dural bridging veins.
Cerebral atrophy (ETOH and elderly patients) causes increased tension on these veins predisposing them to tearing.
Trauma causing the initial bleed may be so mild as to be absent from hx.
Local inflammatory reaction follows the haemorrhage and results in haematoma cavity with membranes within it
Clot liquefies over time and this collection may expand.
This may be as a consequence of recurrent microbleeds from dural capillaries and haematoma membranes, secretion of fluid from haematoma membranes and osmotic fluids shifts into the haematoma cavity
Indications for operative mx of chronic SDH
Presence of neurological deficit
Severe and persistent headache
What are the surgical options for craniotomy
Twist-drill
Burrhole (most common)
Craniotomy
Cx of surgery for SDH
Seizures
Intracranial haematoma
Pneumocephalus
Infection (including subdural empyema)
30% risk of recurrence.
Risk to life with GA
Trauma in the hx of SDH may be absent in what proportion of cases
Up to 50%
SDH recurrence rate
Up to 30%
What are the challenges to treatment of chronic SDH
May be due to multiple bleeds- loculation of haematoma making them harder to drain via single hole.
Elderly population with multiple co-morbidites.
Elderly brains are slower to re-expand and fill the subdural space after the haematoma is evacuated, this space continues to stretch bridging veins and has tendency to fill with blood- reaccumulation.
More common in pts on anticoagulation
Twist drill craniostomy
Can be done under LA.
Small-diameter drill bit and the burrhole drilled without direct vision.
Skin is closed over the burrhole without formal irrigation in the hope that a liquefied haematoma will be absorbed into the galea.
Less invasive but probably less effective
Burrhole drainage
Can be performed under LA.
Operating theatre
Allows formal irrigation of the clot either in and out of a single burrhole or through two.
Burrholes are left open and the haematoma cavity communicates in the subgaleal space.
Santarius et al supports soft subdural catheter use for post-operative drainage for 2/7.
Santarius 2009
Lancet
Drain vs no drain after the burrhole evacuation of chronic SDH.
RCT.
The primary endpoint was recurrence needing redrainage. Trial stopped early. Analyses on the intention to treat.
Recurrence occurred in 9.3% with drain vs 24% without.
Mortality was 8.6 vs 18.1
Medical and surgical complications were much the same.
Craniotomy in SDH
Usually reserved for re-collected SDH or those with loculations that cannot be managed with burrholes alone.
Craniotomy will allow direct visulation of the subdural space and the opportunity to divide or excise the membranes that form the compartments within the haematoma cavity.
Decision to be made in the period post-SDH evacuation
When to let the patient sit up
When to restart anticoagulants
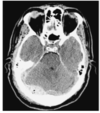
Describe this image and its issues

BIlateral chronic SDH with larger on the left and midline shift to the right.
There will also be vertical shift on the brain.
Bilateral burrholes are required to evacuate both haematomas.
Recurrent chronic subdural haematoma
Patient who has had a chronic subdural haematoma drained returns with scan showing persisting subdural collections.
Can represent new episode
Reaccumultion of fluid
Or simply saline wash.
Can also become infected and present with sepsis +/- worsening headahce or neurological deficit
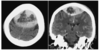
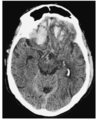
Describe this CT

The arrows show septations within the collection.
There is mass effect causing effacement of the sulci with the right lateral ventricle displaced downwards out of the imaging plane indicating downward brain hernaition.
Little midline shift is evident.
Dexamethasone in SDH
2mg BD may help with conservatively managed SDH- settles headache and some mild neurological deficits.
May work throguh stabilising chronic SDH membrane and protective effect on the cerebral cortex
Mx of VTE in neurosurgical patients
NICE advise mechanical prophylaxis
with LMWH commenced 12-24h post op if risk of major bleeding is low.
If presentation is with cranial or spinal haemorrhage, LMWH is not recommended until the lesions is secured or condition stable
Rates of ICH on aspirin
0.2-0.3%
ICH on aspirin + clopidogrel
0.3-0.4% per year
ICH on warfarin
0.3-1%/year vs 0.15%/year in age matched population
Risk off thromboembolic complications when off warfarin %/year
Metallic heart valve
4-12
Risk off thromboembolic complications when off warfarin %/year
AF
1.9-18.2%