Neuro-oncology Flashcards
(223 cards)
A 68-year-old man collapsed at home. In the emergency department, he was drowsy and dysphasic, with moderate right-sided weakness (MRC grade 4/5). His left pupil was 5mm, the right was 3mm, and both reacted to light. He had attended 2 weeks earlier because of difficulties with his speech.
What is the neurosurgical DDx
The dysphasia and a right hemiparesis suggest a left cerebral lesion. Unequal pupils may indicate impending transtentorial herniation from mass effect. The speech difficulties two weeks earlier suggest a rapidly expanding mass lesion such as a malignant tumour or a subdural haematoma. The reasons for collapse are unclear from the limited history but he may have suffered a seizure.

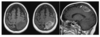
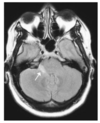
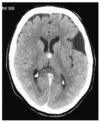
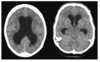
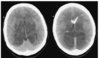
There is a mass in the left hemisphere (A) surrounded by an extensive area of low density (B) which represents oedema. There is midline shift (C) and compartmental hydrocephalus (demonstrated by the enlarged lateral ventricles on the right (D) due to compression of the ventricular system at the foramen of Monro. There is herniation of the uncus of the left temporal lobe seen on the lower slice (E).
What are the three main types of intracerebral oedema
Cytotoxic
Interstitial
Vasogenic
Cytotoxic oedema
Mainly in traumatic and ischaemic brain injury
Results from defective sodium ATP-drive transmembrane channels in affected cells.
Leads to Na and subsequently water retention.
It is not responsive to corticosteroids
Interstitial oedema
Occurs in hydrocephalus and is due to high CSF pressures in ventricular system resulting in CSF egress into adjacent brain parenchyma
Vasogenic oedema
Due to increased capillary permeability from breakdown of BBB, seen principally with tumours and abscesses. Responsive to corticosteroid therapy.
A 68-year-old man collapsed at home. In the emergency department, he was drowsy and dysphasic, with moderate right-sided weakness (MRC grade 4/5). His left pupil was 5mm, the right was 3mm, and both reacted to light. He had attended 2 weeks earlier because of difficulties with his speech.

The mass exhibits ring enhancement. The differential diagnosis is between a highgrade glioma, an abscess, and metastasis. In the absence of raised infective markers, a tumour is more likely
A 68-year-old man collapsed at home. In the emergency department, he was drowsy and dysphasic, with moderate right-sided weakness (MRC grade 4/5). His left pupil was 5mm, the right was 3mm, and both reacted to light. He had attended 2 weeks earlier because of difficulties with his speech.
CT shows likely tumour
Mx

Risk of rapid deterioration due to raised ICP
Corticosteroids to reduce vasogenic tumour oedema and decompressive surgery.
This gentleman underwent craniotomy and debulking of the tumour.
Treatment of glioblastoma after surgical resection
Radiotherapy and temozolomide for patients with good performance status.
Px is 1y even with treatment
Fixed pupil
Suggests compression of CN3 to such an extent that neural transmission has been impeded.
Use of MRI in differentiation of cerebral tumours from abscesses
DWI MRI can be used to differentiate cystic/necrotic tumour from an abscess.
DWI indicates the degree to which water molecules can diffuse out of cells.
It is typically restricted in abscesses, yielding hyperintense signal on DWI. Tends not to be restricted in tumours.
The pattern on the apperent diffusion coefficient sequence is the opposite.
Abscess ring may appear hypointense on DWI a feature not seen in tumours.

Classification of brain tumours
Primary
Secondary
Benign
Malignant
Def: Glioma
Brain tumour that arises from the brain parenchyma
Grading of gliomas
Now based on molecular factors as per WHO classification.
Previously Low grade WHO I+II
High grade WHO III+IV
Glioblastoma is a grade IV glioma that is the most aggressive
Treatment options for glioma
Observation (low grade)
Sx
CTx
RTx
Prognosis variable
Typical primary sites for metastasis to brain
Lung
Kidney
Breast
Melanoma
Colorectal
Def: Meningioma
Typically but not always benign tumours, that arise from the arachnoid cap cells of the meninges
Grading of meningiomas
I benign
II atypical (uncommon)
III malignant (rare)
Locations of meningiomas
Parasagittal
Parafalcine
Convexity
Juxtasellar
Olfactory groove
Posterior fossa
Aetiology of meningiomas
Sporadic but can be familial.
Radiation exposure
NF2
?COCP, obesity
CPA tumours
Vestibular schwannoma
Meningioma
Epidermoid
Ependyoma
Def: Vestibular schwanomma
Beign tumours arising from Schwann cells of the vestibulocochlear nerve
Bilateral schwannomas are seen in?
NF2

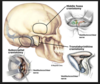
Treatment options for schwannomas
Observation
Sx
retrosigmoid
Translabyrinthine approach
RTx