Vascular Neurosurgery Flashcards
(223 cards)
Name the labelled structures

A- left vertebral artery
B- Right vertebral artery
C- Right anterior inferior cerebellar artery (AICA)
D- Basilar artery
E- Superior cerebellar artery
F- Left posterior cerebral artery
G- Arrowhead on R ICA.
H- L ICA
I- L ICA bifurcation into ACA and MCA
J- Left ACA
K- Left MCA
L- ACA
M- AComm
N- Bifurcation of R MCA
The PICA normally branches off the distal part of the vertebral arteries
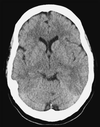
A 64-year-old man presented to the emergency department after experiencing a severe headache which began suddenly when he was watching TV. He felt nauseous and had vomited several times. At hospital, his GCS was 14/15 (E3, V5, M6), and his pupils were equal and reactive, with no focal neurological deficits. He had a history of hyper- tension and his blood pressure was 181/122mmHg.
What is the differential diagnosis, and what investigation should be performed?
The differential diagnosis for a severe sudden onset headache includes any variety of intracranial haemorrhage (subarachnoid haemorrhage (SAH), intracerebral haemorrhage, pituitary apoplexy) and migraine. Intracerebral haemorrhage is usu- ally accompanied by lateralizing signs. A CT scan should be performed urgently to exclude intracranial haemorrhage.
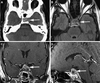
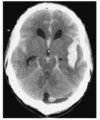
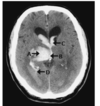
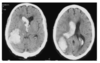
What is the diagnosis
Identify the arrowed features on the scan

SAH with evidence of hydrocephalus
- Blood in sulci
2 + 3: Frontal and occipital horns of the lateral ventricles are dilated as is the third ventricle (4)
There is intraventricular blood (5)
The low-denstry area around the frontal horn represents transependymal flow (6) due to acute hydrocephalus
Blood is seen in the right sylvian fissure, 7, and in the interpeduncular cistern, 8 and the right and left, 9 10, ambient cisterns.
The quadrigeminal cistern 11 is clear of blood.
The temporal horns of the lateral ventricles are dilated
What are the causes of SAH
Trauma
Spontaneous SAH:
Ruptured cerebral aneurysm (70% of cases)
AVM (5-10%)
Vasculitis- e.g. SCD or moyamoya disease
In 15-20% of patients, all investigations including catheter angiography prove negative

In this case the asymmetrical blood distribution is highly suspicious of a ruptured aneurysm on the right middle cerebral, posterior com- municating or internal carotid artery
What are the general measures that need to be instituted for a patient with aneu- rysmal subarachnoid haemorrhage, and what are the specific management issues in this case?
Supportive- optimise cerebral perfusion
Identify the aneurysm and secure it.
General measures in Mx of SAH
Mx in HDU or ICU setting with frequent neuro-obs
Bed rest to minimise fluctuations in BP
Bloods- FBC, electrolytes, clotting, G+S
Analgesia- paracetamol and codeine
Laxatives to reduce straining
DVT prophylaxis with TEDS (LMWH after surgical mx of aneurysm)
Adequate hydration to reduce risk of volume depletion
CXR to exclude neurogenic pulmonary oedema
ECG to detect myocardial damage
Nimodipine for 21/7.
Specific measures to improve cerebral perfusion e,.g. CSF diversion or haematoma evacuation to reduce ICP.
Cerebral angiography to look for aneurysm
Mx of BP in SAH
Patients with SAH often present with raised BP.
The risk of aneurysm rupture should be balanced against the risk of cerebral hypoperfusion.
BP should not be aggressively managemend in the acute setting.
Mx of hydrocephalus in SAH
Immediate CSF diversion
Options for CSF diversion
LP
Lumbar drain
External ventricular drain
(First two are relatively contraindicated in the presence of mass effect or obstructive hydrocephalus)
LP carries lower morbidity.
EVD may be preferrable if there is a high blood load to allow controlled drainage of CSF and if there is intraventricular blood which could block CSF flow through the ventricles.

A- ICA
B- Ophthalmic
C- ACA, A1 segment
D- MCA, M1 segment
E- aneurysm
F- ACA, A2 segment
What are the different patterns of bleeding in aneurysmal SAH
A Sylvian fissure
B Basal cisterns
C Interhemispheric, frontal lobe
D Intraventricular
E Subdural
F Perimesenecephalic
Location of blood- predictiveness of aneurysm site
Location of blood is predictive of site of ruptured aneurysm in around 80% of SAH patients.
Perimesencephalic SAH
Presents as typical SAH but usually less distressed and neurologically disabled.
Angiography is usually normal and bleed is usually considered to be venous e.g. pontine vein
Requiring no further treatment
SAH aneurysm location by site of bleeding:
Sylvian fissure
MCA
SAH aneurysm location by site of bleeding:
Basal cisterns
Basilar artery, SCA, PCom
SAH aneurysm location by site of bleeding:
Interhemispheric. Frontal lobe
ACom, ACA
SAH aneurysm location by site of bleeding:
Intraventricular
ACom (through lamina terminalis)
Basilar artery (through 3rd ventricle)
PICA (through 4th ventricle)
SAH aneurysm location by site of bleeding:
Subdural
PCom, ACom (through arachnoid)
SAH aneurysm location by site of bleeding:
Perimesencephalic
Non arterial e.g. pontine veins
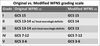
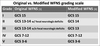
What are the two commonly used scales for SAH grading
Fisher grading (Modified fisher)
WFNS
Features of Fisher grading
Use the amount of blood seen on CT to predict the subsequent risk of radiological vasospasm.
1-4.

Issues with original Fisher grading
Used an early CT scanner with images printed on films. Measured manually with rulers, theefore measurements only apply to images obtained on scanner.
Patients could also be classified into more than one grade
Fisher 1
No blood on CT scan