Paediatric Neurosurgery + Hydrocephalus Flashcards
(117 cards)
A 72-year-old man was referred by the neurologists with a 2-year history of progressive difficulty with mobility. He was previously very active and enjoyed long walks outdoors, but these have been curtailed recently because of a number of falls. On even ground he finds he has slowed and on uneven ground he frequently trips. His wife has become somewhat frustrated with his deterioration. In addition he is reported by his family as being ‘less sharp’ than he used to be and he is no longer able to complete crosswords. They also say he has become forgetful at times. His GP referred him to a neurologist where an MRI scan of the brain was performed (Fig. 53.1 ) and he has been referred for a neurosurgical opinion.
What does the MRI show?

Marked ventricular enlargement. No signal change around the ventricles- chronic process of enlargement.
Should review lower slices to ensure there is no mass lesion or other reason for hydrocephalus
A 72-year-old man was referred by the neurologists with a 2-year history of progressive difficulty with mobility. He was previously very active and enjoyed long walks outdoors, but these have been curtailed recently because of a number of falls. On even ground he finds he has slowed and on uneven ground he frequently trips. His wife has become somewhat frustrated with his deterioration. In addition he is reported by his family as being ‘less sharp’ than he used to be and he is no longer able to complete crosswords. They also say he has become forgetful at times. His GP referred him to a neurologist where an MRI scan of the brain was performed (Fig. 53.1 ) and he has been referred for a neurosurgical opinion.
DDx?

Spinal disease would explain gait but not memory impairment.
In view of MRI diagnosis is either cerebral atrophy and a chronic progressive dementia or chronic hydrocephalus of unknown aetiology (normal pressure hydrocephalus)
Pathophysiology of NPH
?Failure of CSF absoprtion either at the arachnoid granulation or due to poor CSF flow through the subarachnoid space.
If there is reduced wall tension, according to the law of Laplace, the ventricles may be prone to exapnsion even at relatively low pressures.
Hakim’s triad
Ataxia
Dementia
Urinary incontinence
NPH
Urinary incontinence in NPH
Different to the pattern of incontinence in spinal cord lesions (painless retention and overflow)
It is the apparently normal passage of urine in response to a full bladder without patient being aware or concerned by it.
A 72-year-old man was referred by the neurologists with a 2-year history of progressive difficulty with mobility. He was previously very active and enjoyed long walks outdoors, but these have been curtailed recently because of a number of falls. On even ground he finds he has slowed and on uneven ground he frequently trips. His wife has become somewhat frustrated with his deterioration. In addition he is reported by his family as being ‘less sharp’ than he used to be and he is no longer able to complete crosswords. They also say he has become forgetful at times. His GP referred him to a neurologist where an MRI scan of the brain was performed (Fig. 53.1 ) and he has been referred for a neurosurgical opinion.
MRI shows ventriculomegaly
How would you proceed?
DDx is patients with a degenerative neurological condition causing dementia and true NPH.
It can be difciult to differentiate between these two and subsequently to identify those patients who may benefit from CSF diversion.
Hydrocephalus ex vacuo
Cerebral atrophy and subsequent ventricular expansion into the shrinking brain due to reduced wall tension
Possible diagnostic tests in ?NPH
Measurement of CSF pressure by ICP monitoring or LP- if there are B-waves (an ICP pressure of >20mmHg for >5 minutes)
Baseline pressure is usually normal and an absence of B-waves does not exlude the diagnosis.
Therapeutic CSF drainage is an alternative as it will temporarily mimic the action of a shunt. Initial baseline physiotherapy and psychological Ax followed by LP or lumbar drain for 24-48h.
After the post-drainage period the patient should be monitored for improvement in gait (e.g. timed 10m walk) and cognitive function (e.g. repeat MSE)
What is a concern in placing shunts in patients with very large ventricles?
Overdrainge of CSF may produce subdural collections and haematomas
Regulation of CSF pressure in VP shunt
CSF pressure in VP shunt is regulated by the valve.
High pressure valves open only when CSF pressure is high.
Low pressure when CSF is high or normal and close at low pressure.
VP shunts in patients with NPH
Ultimately patients with NPH require the shunts to be open at low pressure though doing so immediately with a shunt risks subdural haematoma.
Solution is to place a variable pressure valve in the shunt that can be adjusted externally.
Initially valve is set at high pressure and progressively lowered.
Theory is to allow the brain to expand gradually rather than for it to collapse quickly.
Cotugno
Credited with discovering CSF
Dandy
Experimental verification of CSF circulation
Components of the ventricular system and CSF circulation
Two lateral paired ventricels
Communicate with third ventricle via the foramen of Munro
Third ventricle-> fourth ventricle via the aqeuduct of Sylvius
Fourth ventricle comunicates with cranial and spinal subarachnoid space via the foramen of Magendie and the paired foramina of Luschka
Secretion of CSF
70% from the choroid plexus but some is derived from capillary ultrafiltrate and metabolic water production
Energy-dependent process (Na/K ATPase) with sodium being secreted in to subarachnoid space and water following it
Rate of CSF production /day
450mL/day
Total volume of CSF
150ml with 25mL in the ventricular system (remainder is in the spinal canal and subarachnoid space)
Location of choroid plexus
Floor, body and roof othe temporal horns of the lateral ventricles
Roof of third ventricle
WIthin the fourth ventricle
Composition of the choroid plexus
Single layer of cuboidal epithelial cells surrounding blood capillaries.
Absorption of CSF
Arachnoid granulations in the superior sagittal sinus.
Operates a pressure-dependent valve, transmitting CSF when the ICP>venous presssure.
Some CSF is also absorbed by veins.
Rate of absorption regulates CSF pressure and production is relatively constant.
Reduction of CSF production
Decreased by carbonic anhydrase inhibitors (acetazolamide) and noradrenaline.
Increased by CO2 and volatile anaesthetics
What part of the brain regulates CSF production
Raphe nuclei
Def: hydrocephalus
Results from an imbalance between production and absorption of CSF resulting in increased CSF volume and pressure.
Must be distinguished from ventriculomegaly (i.e. dilated ventricles with low or normal CSF pressure) and NPH.
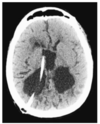
Characteristic of acute hydrocephalus on neuroimaging
Periventricular lucency typically at the tips of the frontal horns of the lateral ventricles.
This represents CSF egress into the adjacent white matter and indicates high intraventricular pressure