Haematology 1 - Acute leukaemia Flashcards
(27 cards)
What is the median age of presentation of AML?
65-70
↑ prevalance with age (ex ALL (i.e. TAM in Down’s syndrome is an AML))
In which type of acute leukaemia are duplication abnormalities most common?
AML
trisomy 8 and trisomy 21 (predisposition to AML - TAM in Down’s syndrome)
What type of leukaemia is associated with chromosome loss and part-deletion
AML - del (5q) or del (7q)
What do chromosomal inversions or translocations lead to?
new fusion genes (ALL and AML) or abnormally regulates (mainly ALL)
Acute Myeloid Leukaemia / AML; t (8; 21) → RUNX1+RUNX1T1
Core Binding Factor – AML / CBF-AML; Inv (16), t (16; 16) → fusion gene. Partial block – some mature ‘eosinophil-type’ cells remain
Acute Promyelocytic Leukaemia / APML; t (15; 17), PML-RARA
AML type 1 vs type 2 abnormalities
Type 1 - promote prolfieration and survival (anti-apoptosis)
Type 2 - block differentiation (would normally be follow by apoptosis) -> blast accumulation

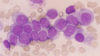
What would blood film show in AML?
uniform population of blast cells
Give an example of disrupted transcriptor function in AML
core binding factor
t(8; 21) - RUNX1 fusion with RUNX1T1
inv(16) - CBFB fusion with MYH11
What is the key triad of clinical features of AML?
Anaemia
Thrombocytopaenia
Neutropaenia
Also local infiltration -> hepatosplenomegaly, gum infiltration, skin/CNS infiltration, lymhpadenopathy
Recall some clinical signs that can be used to identify AML
Hepatosplenomegaly
Monocytic gum infiltration
CNS disease
Occasional lymphadenopathy
What is the most effective investigation for differentiating AML and ALL, and what results would it show for each?
Immunophenotyping:
Don’t need to know details:
AML: CD13/1/15
ALL: CD3/4/18/19/20
How can myeloid lineage be proved on blood film?
Presence of auer rods
What are some cytochemical stains used in AML?
Myeloperoxidase stain (enzyme present in myeloid cells)
Sudan Black stain
Non-specific esterase stain
What cytological differences would you see in ALL vs AML
AML - granules and Auer rods, circulating blast cells
R sided - cannot determine → cytochemistry
Recall some useful supportive therapies for AML
Blood products: red cells, platelets and FFP
Antibiotics
Long line
Allopurinol (as uric acid may be released from dying cells when treatment is started)
Recall some targeted molecular therapies that can be used for AML treatment
APML = All-trans-retinoic acid (ATRA) and AO
Ph +ve (CML, but also rare AML cases) = tyrosine kinase inhibitors
Biologics = anti-CD33 antibody linked to cytotoxic antibody (e.g. gemtuzumab)
Recall the pathophysiolgy of APML
excess of abnormal promyelocytes (Auer rods) → sudden DIC
Classical vs variant APML
Classical - blast cells with Auer rods and granules
Variant - finer granules, bilobed nuclei

What mutation is responsible for APML?
t (15; 17) → PML-RARA fusion gene
Most patient can be cured as molecular mechanism understood
Which type of leukaemia is most likely to cause haemorrhage?
Acute Promyelocytic leukaemia (APML)
Which type of leukaemia is most likely to cause DIC?
APML
Which type of leukaemia is most likely to present with long bone pain?
ALL
What are some poor prognostic indicators of ALL?
t(4;11) Hypodiploidy
What are some good prognostic indicators for ALL?
Hyperdiploidy t(12;21) t(1;19)
TK inhibitors (Ph +ve; t(9; 22)
Recall some sights of leukaemic involvement in ALL that you wouldnt see in AML
Thymus, testes, CNS
these are ‘sanctuary sites’ as chemotherapy cannot reach them easily


