Microbiology 3 - Antimicrobial Agents 2 Flashcards
(17 cards)
What is MIC?
minimum inhibitory concentration
minimum [drug] required to inhibit growth of organism in a culture
What is the Minimum Inhibitory Concentration and Breakpoint of an antibiotic useful for?
Working out sensitivity
MIC > breakpoint = resistant
MIC < breakpoint = sensitive
what Abx are optimal for nonsocomial infections and severe sepsis?
broad spec Abx higher survival rates
Tazocin/ceftriaxone, metronidazole +/- gentamicin
Neutropoenic: Tazocin + gentamicin
What antibiotic should be given for gram pos cocci in clusters?
Flucloxacillin
What antibiotic should be given empirically for gram neg cocci?
Ceftriaxone (could be meningococcus)
What is the “eagle effect”?
Increasing the penicillin dose –> decreasing antibacterial activitity after a point
How does the choice of antibiotic to treat UTI differ between community and hospital?
Community: nitrofurantoin/ trimethoprim
Hospital: cephalexin/ augmentin
When would you switch from IV to oral Abx?
most infections if patient stabilised after 48 hours of IV treatment
CNS infections and severe infections such as osteomyelitis and endocarditis you may NOT switch to PO
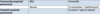
type 1vs2vs3 Abx Pharmacokinetics/Pharmacodynamics
- Peak above MIC (Cmax) = MOST IMPORTANT factor (concentration-dependent effects) = ONE BIG DOSE
- time-dependent → maximise time above MIC = frequent dosing
- Sort of a combination of Type I and Type II
The AUC above the MIC is the MOST IMPORTANT factor (both concentration and time-dependent effects)

Which Abx would you use against N. meningitidis meningitis
Ceftriaxone
7 days
(amox if listeria – young/old)
Whic Abx against skin infection S. aureus?
Flucloxacillin (unless allergy)
Which Abx against β-haemolytic Streptococcus pharyngitis ?
Benzylpenicillin 10 days
Which Abx against pneumonia?
Which Abx against UTI?
Simple - 3 days

Which Abx should be given in C Diff?
Stop ceph
Metronidazole (PO)
VAncomycin (PO)
If E coli is fully susceptible which is the narrowest spectrum Abx to use?
amoxicillin - but often resistant so use if susceptible


