Immunology 3 - Transplantation Flashcards
(30 cards)
Recall the 3 phases of immune response to a transplanted graft
- Recognition of foreign antigens
- Activation of antigen-specific lymphocytes
- Effector phase of grant rejection
What are the 2 most variant protein variants in clinical transplantation?
ABO blood group HLA antigens (Ch6 HLA)
On which type of cell is HLA class I (A/B/C) expressed?
All cells
On which type of cell is HLA class II (DR/DQ/DP) expressed?
Antigen-presenting cells
Which types of HLA fall into each class?
HLA-A, B, C = class 1 HLA-DR, DQ, DP =class 2
Most impt - DR>B>A
Which part of the HLA molecule is highly variable?
peptide binding grove - allows us to present variety of Ag to immune cells
HLA I - ⍺1+⍺2
HLA II - ⍺1

In T cell-mediated transplant reaction, how are alloreactive T cells activated (phase 1)?
- Presentation of foreign HLA antigens in MHC by APCs (both DONOR and HOST APC cells are involved)
Direct - donor APC present Ag to T cells (mainly acute rejection)
Indirect - recipient APC presents donor Ag to T cells (mainly chronic)
- Costimulatory signals
occurs in lymph nodes
What are the actions of activated T cells in T cell-mediated transplant rejection?
- Proliferation
- Produce cytokines (especially IL2)
- ‘Help’ CD8+ cells
- ‘Help’ antibody production
- Recruit phagocytic cells
How does T cell mediated rejection result in graft damage
Cytotoxic T cells: granzyme B, perforin, Fas-ligand
Macrophages: phagocytosis, proteolytic enzymes, cytokines, O2/N2 radicals
What test can be used to see if transplant rejection is occurring?
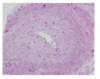
A biopsy - an inflammatory response will be seen

What are the key histological features of T cell-mediated transplant rejection?
Lymphocytic interstitial infiltration
Ruptured tubular basement membrane
Tubulitis (inflammatory cells within tubular epithelium)
Macrophages, recruited by T cells
arteritis
What are some examples of drugs targeting T cell rejection?
- Steroids
- Inhibitors of cell signalling / Calcineurin inhibitors (i.e. Tacrolimus, Cyclosporine)
- Anti-proliferative agents (i.e. Mycophenolate mofetil, Azathioprine)
- Inhibitors of cell surface receptors (i.e. Anti-CD3 antibody (OKT3), ATG / Anti-thymocyte globulin)
- Alemtuzumab: anti-CD52 monoclonal antibody that causes lysis of T cells
- Basiliximab: anti-CD25 monoclonal antibody which targets IL-2-R → less proliferation
Recall the 3 phases of antibody mediated rejection
- B cells recognise foreign HLA
- Proliferation and maturation of B cells with anti-HLA antibody production
- Effector phase: antibodies bind to graft ENDOTHELIUM (intravascular disease)
Recall the process of antibody-mediated rejection phase 3
Abs bind HLA on graft vacular endothelium –> complement activation to form MAC and inflammatory cell recruitment
endothelial injury and inflammation (capillaritis)
Capillaritis is a cardinal feature of antibody-mediated rejection
What are the key histological features of antibody-mediated transplant rejection?
- Capillaritis = inflammatory cells in capillaries of the kidney → injury
- also procoagulant tendencies and closure of microcirculation → graft fibrosis
- Immunohistochemistry shows fixation or complement fragments on endothelial cell surfaces

What is the main difference between T cell and B cell mediated rejection?
T cells = interstitial damage, B cells = endothelial damage
What test is used to do ABO/HLA typing before a transplant?
PCR-DNA sequencing
NOTE: mismatch positive transplantation CAN take place, but requires a lot of preparation (plasma exchange and IVIG)
What at the 3 methods of screening for anti-HLA antibodies?
- Cytotoxicity assays - does recipient serum kill donor’s lymphocytes? (+ve crossmatch → cell lysis (i.e. +ve is bad)
- Flow cytometry - does recipient’s serum bind donor’s lymphocytes? looking for BOUND FLUORESCENTLY-LABELLED ANTIBODY
- Solid phase assays, beads contain all possible HLA phenotypes - fluorescent Ig to determine which HLA epitopes bind Abs
What is the most reliable HLA test nowadays?
Solid phase assays - uses beads that have different HLA epitopes and fluorescent colour
Recall 2 treatments that all transplant recipients receive to prevent rejection?
Induction agent + baseline immunosuppression
What are some examples of baseline immunosuppression for transplants?
- Mycophenalate mofetil/azathioprine
- Tacrolimus (calcineurin inhibitor)
- +/-Prednisolone
- (Pre-Transplant Meds = acronym)
(impt - come up)
What are some examples of induction agents in transplant immunosuppression?
T cell depleting - OKT3/ATG, anti-CD52
anti- IL2 R
How would you nonitor transplant function?
creatinine
if ↑creatinine - take biopsy and classify rejection
A pt has an episode of acute T cell-mediated rejection 2 months post-transplantation. What would be the most common drug administered?
Corticosteroids - pred
ATG/OKT3