Haematology 14 - Blood Transfusion 1 & 2 Flashcards
(75 cards)
Outline which Abs and Ags are present in groups A/B/AB/O
What subtype of antibody determines ABO group?
IgM Abs in plasma - reacts against normal RBC Ags
(IgG against atypical RBC Ags)
What happens if you give ABO incompatible blood?
massive intravascular haemolysis → fatal
Which blood type can RhD + or - receive?
- RhD +ve (85%) - RhD positive and RhD negative (but waste)
- RhD -ve (15%) - RhD neg ONLY
What happens if you give RhD pos blood to RhD neg pt?
make anti-D Abs (IgG)
delayed haemolytic transfusion (NOT direct agglutination so not immediate haemolysis)
IgG - cause a DELAYED transfusion reaction; extravascular haemolysis
As opposed to naturally occurring IgM antibodies (that cause an IMMEDIATE intravascular haemolysis)
will be picked up by the lab next time they need blood
What happens if RhD + blood is given to RhD - mother ?
→ HDN or severe foetal anaemia and heart failure (hydrops fetalis)
IgG can cross placenta
Group and screen vs full crossmatch
GROUP and SCREEN– check ABO group and plasma antibodies in patient
Full crossmatch– checks patient’s blood against donor blood specifically
Recall 2 ways in which patients’ blood group is tested
- ‘forward group’ - known anti-A,B and O reagents against patient’s RBCs
- ‘reverse group’ - known A and B group RBCs against the patient’s plasma (IgM Abs)
Describe the process of antibody testing of blood
Group and screen
- Use 2 or 3 reagent RBCs containing all important RBC Ags
- Then incubate the patient’s plasma using the indirect antiglobulin technique (IAT)
Anti-Human Globulin (AHG) promotes agglutination -bridges RBCs coated by IgG (which can’t themselves bridge 2 RBCs)

How is IAT technique used in full crossmatching?
patient plasma incubated with donor RBCs
detects Ab-Ag reaction → destroys RBCs → extravasc haemolysis
Add antiglobulin reagent to promote cross-linking
What is the purpose of ‘immediate spin’ blood testing?
Full cross match
Used in emergencies only
Incubation for just 5 minutes
Determines ABO compatibility only
What are the 3 pillars of patient blood management?
- Optomise haematopoiesis
- Reduce bleeding (eg stop anti-platelt drugs, cell-salvage techniques)
- Harness and optomise physiological tolerance of anaemia

For which blood products is D compatibility required?
Red cells and platelets (but not FFP or cryoprecipitate)
What is the storage temperature of red cells, platelets, FFP and cryoprecipitate?
Red cells: 4 degrees C
Platelets: 20 degrees C
FFP: frozen - 4 degrees C once thawed
Cryoprecipitate: Room temp once thawed
What is the storage length of red cells, platelets, FFP and cryoprecipitate?
Red cells: 35 days
Platelets: 7 days
FFP: 24 hours
Cryoprecipitate: 4 hours
What is the transfusion rate of red cells, platelets, FFP and cryoprecipitate?
Red cells: 1 unit over 2-3 hours
Platelets: 1 unit over 20-30 mins
FFP: 1 unit over 20-30 mins
Cryoprecipitate: 1 unit over 20-30 mins
Why must platelets be given quicky?
stored at room temp so bacteria can contaminate it quickly
if pt fever → stop platelets and culture
send platelets back to lab for microbiological testing
what type of reaction if more likey with plasma transfusion?
allergic - plasma frozen so unlikely to be contaminated by microbes
How much blood loss counts as ‘major’?
>30% blood volume lost
How low does haemaglobin need to be to require transfusion peri-operatively vs post-chemo?
Peri-op/ crit care: <70g/dL
Post-chemo: <80g/dL
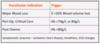
Indications for RBC transfusion
When are platelets contra-indicated?
TTP/ heparin-induced TTP
Indications for platelet transfusion

When is FFP indicated?
Contains all the clotting factors
Adult dose = 15 mL/kg (1 unit of FFP contains 250 mL à enough for 16.6kg)




